Mi-Suk Kang Dufour PhD, MPH
- Associate Adjunct Professor, Biostatistics

https://publichealth.berkeley.edu/people/mi-suk-kang-dufour/
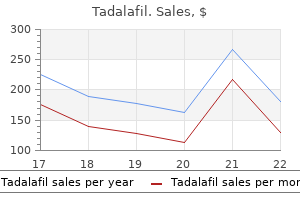
Note: Home dialysis clients usually are monitored by conven tional dialysis center or interdisciplinary team impotence over 40 purchase generic tadalafil line. Sources for supplies when away from home Home dialysis clients are often capable of travel icd 9 code for erectile dysfunction due to medication order 2.5mg tadalafil amex, even overseas erectile dysfunction treatment in rawalpindi buy tadalafil without prescription, with proper preplanning and support erectile dysfunction caused by radiation therapy buy tadalafil 2.5 mg lowest price. Refer to Renal Dialysis: Peritoneal impotence age 45 buy tadalafil from india, below erectile dysfunction treatment after prostatectomy purchase tadalafil cheap, or Hemodialysis, to complete the plan of care. Requires a surgically placed abdominal catheter and uses dwell time because, as dextrose in the solution crosses the peritoneum to lter toxins and excess uid from the into body, it becomes glucose and starts to draw uid body from the peritoneal cavity back into the body, thereby b. Fluid removal is controlled by adjusting the dextrose reducing the efficiency of the exchange and requiring a concentration in the dialysate. May be preferred over hemodialysis because it uses a daytime cycle with solution in abdomen simpler technique and provides more gradual physiological 2. May be method of choice for younger individuals changes engaged in school or work activities d. Manual single-bag method is usually done as an inpatient remaining renal function procedure with short dwell times of only 30 to 40 minutes 2. May improve uremia-associated sleep apnea and is repeated until desired effects achieved. A positive balance with more uid in than out indicates need for further evaluation. Record serial weights, compare with intake and output (I&O) Serial body weights are an accurate indicator of uid volume balance. A positive uid balance with an increase in weight providing a consistent reference point. Note Slowing of ow rate or presence of brin suggests partial presence of brin strings or plugs. Anchor Improper functioning of equipment may result in retained uid catheter so that adequate in ow and out ow is achieved. Turn from side to side, elevate the head of the bed, and apply May enhance out ow of uid when catheter is malpositioned gentle pressure to the abdomen. Note abdominal distention associated with decreased bowel Bowel distention or constipation may impede out ow of effiuent. Assess heart and breath bounding pulses, neck vein distention, and peripheral sounds, noting S3 and crackles and rhonchi. Evaluate development of tachypnea, dyspnea, and increased Abdominal distention or diaphragmatic elevation may cause respiratory effort. Assess for headache, muscle cramps, mental confusion, and Symptoms suggest hyponatremia or water intoxication. Changes may be needed in the glucose or sodium concentra tion to facilitate efficient dialysis. Hypernatremia may be present, although serum levels may re ect dilutional effect of uid volume overload. Add heparin to initial dialysis runs; assist with irrigation of May be useful in preventing brin clot formation, which can catheter with heparinized saline. Between dialysis treatments, uids accumulate in the body, particularly in the heart, lungs, and ankles. Therefore, most nephrologists recommend restricting uid to about 1,500 mL/day (Leydig, 2005). Weigh when abdomen is empty, following initial 6 to 10 runs, Detects rate of uid removal by comparison with baseline then as indicated. Inspect mucous membranes, evaluate skin turgor, peripheral Dry mucous membranes, poor skin turgor, and diminished pulses pulses, and capillary re ll. Collaborative Monitor laboratory studies, as indicated, such as: Serum sodium and glucose levels Hypertonic solutions may cause hypernatremia by removing more water than sodium. In addition, dextrose may be absorbed from the dialysate, thereby elevating serum glucose. Note presence of fecal material in dialysate effiuent or strong Suggests bowel perforation with mixing of dialysate and urge to defecate, accompanied by severe, watery diarrhea. Note reports of intense urge to void or large urine output Suggests bladder perforation with dialysate leaking into blad following initiation of dialysis run. Stop dialysis if there is evidence of bowel or bladder perforation, Prompt action will prevent further injury. Demonstrate relaxed posture and facial expression; be able to sleep and rest appropriately. Explain that initial discomfort usually subsides after the rst Information may reduce anxiety and promote relaxation few exchanges. Monitor for pain that begins during in ow and continues during Pain will occur if acidic dialysate causes chemical irritation of equilibration phase. Note reports of discomfort that are most pronounced near the Likely the result of abdominal distention from dialysate. Inadvertent introduction of air into the abdomen irritates the Note report of pain in area of shoulder blade. This type of discomfort may also be reported during initiation of therapy or during infusions and usually is related to stretching or irritation of the diaphragm with abdominal distention. Position changes and gentle massage may relieve abdominal Provide back care and tissue massage. Warming the solution increases the rate of urea removal by dilat ing peritoneal vessels. Cold dialysate causes vasoconstriction, which can cause discomfort and excessively lower the core body temperature, precipitating cardiac arrest. Monitor for severe or continuous abdominal pain and tempera May indicate developing peritonitis. Change dressings as indicated, being careful not to dislodge Moist environment promotes bacterial growth. Note character, color, odor, or drainage from drainage at insertion site suggests presence of local infection, insertion site. Apply povidone-iodine (Betadine) barrier in distal, clamped Reduces risk of bacterial entry through catheter between portion of catheter when intermittent dialysis therapy used. Investigate reports of nausea or vomiting, increased or severe Signs and symptoms suggesting peritonitis, requiring prompt abdominal pain, rebound tenderness, or fever. Obtain specimens of blood, effiuent, and drainage from Identi es types of organism(s) present and in uences choice insertion site, as indicated, for culture and sensitivity. Reduce infusion rate if Tachypnea, dyspnea, shortness of breath, and shallow dyspnea is present. Auscultate lungs, noting decreased, absent, or adventitious Decreased areas of ventilation suggest presence of atelectasis, breath sounds, such as crackles, wheezes, and rhonchi. Client is susceptible to pulmonary infections as a result of depressed cough re ex and respiratory effort, increased viscosity of secretions, as well as altered immune response and chronic, debilitating disease. Promote Facilitates chest expansion and ventilation and mobilization of deep-breathing exercises and coughing. Continuous venovenous hemo ltration via ultra ltration can perform home hemodialysis, if appropriate and convection ii. Cost: Estimates vary from $35,000 to $60,000 annually per procedure, or six to seven times per week for 1. Bruit is the sound caused by the turbulence of arterial blood entering the venous system and should be audible by stethoscope, although may be very faint. If the bruit gets higher in pitch, it could mean narrowing of the blood vessels; if it stops, clot may have formed. Note color of blood and obvious separation of cells and Change of color from uniform medium red to dark purplish red serum. Very dark reddish-black blood next to clear yellow uid indicates full clot formation. Because heparin remains active in the body for 4 to 6 hours, the client is at risk for hemorrhage during and immediately after dialysis (Leydig 2005). Notify physician and initiate declotting procedure if there is Rapid intervention may save access; however, declotting must evidence of loss of shunt patency. Evaluate reports of pain, numbness, and tingling; note May indicate inadequate blood supply. Avoid trauma to shunt; for example, handle tubing gently and Decreases risks of clotting and disconnection. Instruct client not to sleep on side with shunt or carry packages, books, or purse on affected extremity. Have tourniquet Prevents massive blood loss while awaiting medical assistance available. If cannulae separate, clamp the arterial cannula if cannula separates or shunt is dislodged. If tubing comes out of vessel, clamp cannula that is still in place and apply direct pressure to bleeding site. Infection Assess skin around vascular access, noting redness, swelling, Signs of local infection, which can progress to sepsis if local warmth, exudate, and tenderness. Use aseptic technique and Prevents introduction of organisms that may cause infection. Note presence of fever, chills, and Signs of infection or sepsis requiring prompt medical hypotension. Administer medications, as indicated, for example: Lowdose heparin Infused on arterial side of lter to prevent clotting in the lter without systemic side effects. Have client Aids in evaluating uid status, especially when compared with keep diary. Note: Urine output is an inaccurate evaluation of renal function in dialysis clients. Some individuals have water output with little renal clearance of toxins, whereas others have oliguria or anuria. Weight loss over precisely measured time is a measure of ultra ltration and uid removal. Dry weight determines how much excess uid has been removed and serves as a guide for subsequent dialysis run time and solution. Minimizes stress on cannula insertion site to reduce inadver tent dislodgement and bleeding from site. Place client in a supine or Trendelenburg position, as Maximizes venous return if hypotension occurs. Assess for oozing or frank bleeding at access site, mucous Systemic heparinization during dialysis prolongs clotting times membranes, or incisions and wounds. Hematest stools or and places client at risk for bleeding, especially during the any drainage. Serum electrolytes and pH Imbalances may require changes in the dialysate solution or supplemental replacement to achieve balance. Use of heparin to prevent clotting in blood lines and hemo lter alters coagulation and potentiates active bleeding. Volume expanders, such as albumin Volume expanders may be required during or following hemodialysis if sudden or marked hypotension occurs. Reduces the amount of water being removed and may correct hypotension or hypovolemia. May be needed to return clotting times to normal or if heparin rebound occurs within 16 hours after hemodialysis. Restrict sodium intake, as High sodium levels are associated with uid overload, edema, indicated. Restrict uid intake as indicated, spacing allowed uids the intermittent nature of hemodialysis results in uid reten throughout a 24-hour period. Neurogenic bladder, such as may occur following spinal usually using part of the digestive tract cord injury b. Continent urinary diversions bladder cancer were reported in the United States; male-to 1. Mortality: Rate is reportedly 1% to 3% for radical cystecto my, often associated with advanced age and comorbidities (Lohr & Sherk, 2004). Neobladder: Most closely resembles the normal urinary Colonic conduit: Similar to an ileal conduit, but uses a anatomy by using a section of intestine to form a pouch segment of colon instead of ileum. The client is able to urinate pouch or reservoir created inside the body from a spontaneously using abdominal muscles to push the section of stomach or small or large intestine. A stoma urine through the urethra to void; however, intermittent may or may not be required. Ileal conduit: Ureters are anastomosed to a segment of Peristomal: Skin around and closest to the stoma. The proximal section is closed, and ostomy care, is the segment of bowel or ureter brought to the distal end is brought through an opening in the skin the surface of the abdomen. Incontinent or noncontinent urinary diversions: Urine Ureterostomy: the ureter(s) is brought directly through the ows through ureters directly anastomosed to the abdominal wall to form its own stoma. Most commonly, a conduit is created from a collecting device through a permanent stoma. Interrupted anastomosis: Loss of the surgical connection the open end of the conduit is brought to the abdomen of two hollow organs. Cancer, page 846 Peritonitis, page 349 Psychosocial aspects of care, page 749 Surgical intervention, page 782 Client Assessment Database Data depend on underlying problem, duration, and severity, for example, malignant bladder tumor, congenital malformations, trauma, chronic infections, or intractable incontinence due to injury or disease of other body systems, such as with multiple sclerosis. Identi es X-ray examination and uoroscopic visualization of the lling defects caused by tumors or other obstructive disorders.
Payment is dependent on the certification of the plan of care rather than the order zantac causes erectile dysfunction order cheap tadalafil line, but the use of an order is prudent to determine that a physician is involved in care and available to certify the plan erectile dysfunction at 20 discount tadalafil 5 mg without a prescription. The plan erectile dysfunction leakage 10 mg tadalafil free shipping, (also known as a plan of care or plan of treatment) must be established before treatment is begun does erectile dysfunction get worse with age order tadalafil 20mg with mastercard. The evaluation and treatment may occur and are both billable either on the same day or at subsequent visits erectile dysfunction protocol does it work order cheap tadalafil. Therapy may be initiated by qualified professionals or qualified personnel based on a dictated plan erectile dysfunction homeopathic buy tadalafil 10 mg with visa. Treatment may begin before the plan is committed to writing only if the treatment is performed or supervised by the same clinician who establishes the plan. The Treatment Notes continue to require timed code treatment minutes and total treatment time and need not be separated by plan. Progress Reports should be combined if it is possible to make clear that the goals for each plan are addressed. The plan of care shall be consistent with the related evaluation, which may be attached and is considered incorporated into the plan. The plan should strive to provide treatment in the most efficient and effective manner, balancing the best achievable outcome with the appropriate resources. Long term treatment goals should be developed for the entire episode of care in the current setting. When the episode is anticipated to be long enough to require more than one certification, the long term goals may be specific to the part of the episode that is being certified. When episodes in the setting are short, measurable goals may not be achievable; documentation should state the clinical reasons progress cannot be shown. When more than one discipline is treating a patient, each must establish a diagnosis, goals, etc. However, the form of the plan and the number of plans incorporated into one document are not limited as long as the required information is present and related to each discipline separately. For example, a physical therapist may not provide services under an occupational therapist plan of care. However, both may be treating the patient for the same condition at different times in the same day for goals consistent with their own scope of practice. The amount of treatment refers to the number of times in a day the type of treatment will be provided. The frequency refers to the number of times in a week the type of treatment is provided. If the episode of care is anticipated to extend beyond the 90 calendar day limit for certification of a plan, it is desirable, although not required, that the clinician also estimate the duration of the entire episode of care in this setting. The frequency or duration of the treatment may not be used alone to determine medical necessity, but they should be considered with other factors such as condition, progress, and treatment type to provide the most effective and efficient means to achieve the patientsgoals. For example, it may be clinically appropriate, medically necessary, most efficient and effective to provide short term intensive treatment or longer term and less frequent treatment depending on the individualsneeds. It may be appropriate for therapists to taper the frequency of visits as the patient progresses toward an independent or caregiver assisted self management program with the intent of improving outcomes and limiting treatment time. For example, treatment may be provided 3 times a week for 2 weeks, then 2 times a week for the next 2 weeks, then once a week for the last 2 weeks. When tapered frequency is planned, the exact number of treatments per frequency level is not required to be projected in the plan, because the changes should be made based on assessment of daily progress. For example, amount, frequency and duration may be documented as once daily, 3 times a week tapered to once a week over 6 weeks. The clinician should consider any comorbidities, tissue healing, the ability of the patient and/or caregiver to do more independent self management as treatment progresses, and any other factors related to frequency and duration of treatment. It is anticipated that clinicians may choose to make their plans more specific, in accordance with good practice. For example, they may include these optional elements: short term goals, goals and duration for the current episode of care, specific treatment interventions, procedures, modalities or techniques and the amount of each. Also, notations in the medical record of beginning date for the plan are recommended but not required to assist Medicare contractors in determining the dates of services for which the plan was effective. A change in long-term goals, (for example if a new condition was to be treated) would be a significant change. Method and Disposition of Certifications Certification requires a dated signature on the plan of care or some other document that indicates approval of the plan of care. Since delayed certification is allowed, the date the certification is signed is important only to determine if it is timely or delayed. The format of all certifications and recertifications and the method by which they are obtained is determined by the individual facility and/or practitioner. For example, if during the course of treatment under a certified plan of care a physician sends an order for continued treatment for 2 more weeks, contractors shall accept the order as certification of continued treatment for 2 weeks under the same plan of care. If the new certification is for less treatment than previously planned and certified, this new certification takes the place of any previous certification. At the end of the 2 weeks of treatment (which might extend more than 2 calendar weeks from the date the order/certification was signed) another certification would be required if further treatment was documented as medically necessary. The certification should be retained in the clinical record and available if requested by the contractor. Since payment may be denied if a physician does not certify the plan, the therapist should forward the plan to the physician as soon as it is established. Evidence of diligence in providing the plan to the physician may be considered by the Medicare contractor during review in the event of a delayed certification. If the order to certify is verbal, it must be followed within 14 days by a signature to be timely. Recertification is not required if the duration of the initially certified plan of care is more than the duration (length) of the entire episode of treatment. Certifications signed on or after January 1, 2008, follow the rules in this section. Certifications signed on or prior to December 31, 2007, follow the rule in effect at that time, which required recertification every 30 calendar days. Payment and coverage conditions require that the plan must be reviewed, as often as necessary but at least whenever it is certified or recertified to complete the certification requirements. Recertifications that document the need for continued or modified therapy should be signed whenever the need for a significant modification of the plan becomes evident, or at least every 90 days after initiation of treatment under that plan, unless they are delayed. It is possible that patients will be discharged by the therapist before the end of the estimated treatment duration because some will improve faster than estimated and/or some were successfully progressed to an independent home program. After that date, services will not be considered reasonable and necessary due to lack of a certified plan. Certifications and recertifications by doctors of podiatric medicine must be consistent with the scope of the professional services provided by a doctor of podiatric medicine as authorized by applicable state law. Certifications are timely when the initial certification (or certification of a significantly modified plan of care) is dated within 30 calendar days of the initial treatment under that plan. Recertification is timely when dated during the duration of the initial plan of care or within 90 calendar days of the initial treatment under that plan, whichever is less. Certifications are acceptable without justification for 30 days after they are due. Delayed certification should include one or more certifications or recertifications on a single signed and dated document. Delayed certifications should include any evidence the provider or supplier considers necessary to justify the delay. For example, a certification may be delayed because the physician did not sign it, or the original was lost. In the case of a long delayed certification (over 6 months), the provider or supplier may choose to submit with the delayed certification some other documentation. Such documentation may be requested by the contractor for delayed certifications if it is required for review. It is not intended that needed therapy be stopped or denied when certification is delayed. If a certified plan of care ends March 30 and a new plan of care for th th continued treatment after March 30 is developed or signed by a therapist on April 15 and that plan is subsequently certified, that certification may be considered delayed and th acceptable effective from the first treatment date after March 30 for the frequency and duration as described in the plan. Of course, documentation should continue to indicate that therapy during the delay is medically necessary, as it would for any treatment. Denials Due to Certification Denial for payment that is based on absence of certification is a technical denial, which means a statutory requirement has not been met. If an appropriate certification is later produced, the denial shall be overturned. For that reason, it is recommended that the patient be made aware of the need for certification and the consequences of its absence. A technical denial decision may be reopened by the contractor or reversed on appeal as appropriate, if delayed certification is later produced. However, since the inpatients of one institution may be considered the outpatients of another institution, all providers of therapy services may furnish such services to inpatients of another health facility. A certified distinct part of an institution is considered to be a separate institution from a nonparticipating part of the institution. Consequently, the certified distinct part may render covered therapy services to the inpatients of the noncertified part of the institution or to outpatients. Therapy services are payable when furnished in the home at the same physician fee schedule payments as in other outpatient settings. Additional expenses incurred by providers due to travel to a person who is not homebound will not be covered. Under the Medicare law, there is no authority to require a provider to furnish a type of service. However, if the provider chooses to furnish a particular service, it may not charge any individual or other person for items or services for which the individual is entitled to have payment made under the program because it is bound by its agreement with Medicare. General To be covered, services must be skilled therapy services as described in this chapter and be rendered under the conditions specified. Services provided by professionals or personnel who do not meet the qualification standards, and services by qualified people that are not appropriate to the setting or conditions are unskilled services. Unskilled services are palliative procedures that are repetitive or reinforce previously learned skills, or maintain function after a maintenance program has been developed. Services which do not meet the requirements for covered therapy services in Medicare manuals are not payable using codes and descriptions for therapy services. For example, services related to activities for the general good and welfare of patients. Also, services not provided under a therapy plan of care, or are provided by staff who are not qualified or appropriately supervised, are not covered or payable therapy services. Examples of coverage policies that apply to all outpatient therapy claims are in this chapter, in Pub. Further details on documenting reasonable and necessary services are found in section 220. Reasonable and Necessary To be considered reasonable and necessary the following conditions must each be met. Services that do not require the performance or supervision of a therapist are not skilled and are not considered reasonable or necessary therapy services, even if they are performed or supervised by a qualified professional. However, this presumption is rebuttable, and, if in the course of processing claims it finds that services are not being furnished under proper supervision, it shall deny the claim and bring this matter to the attention of the Division of Survey and Certification of the Regional Office. The key issue is whether the skills of a therapist are needed to treat the illness or injury, or whether the services can be carried out by nonskilled personnel. The contractor shall consult local professionals or the state or national therapy associations in the development of any utilization guidelines. The concept of rehabilitative therapy includes recovery or improvement in function and, when possible, restoration to a previous level of health and well-being. Therefore, evaluation, re-evaluation and assessment documented in the Progress Report should describe objective measurements which, when compared, show improvements in function, or decrease in severity, or rationalization for an optimistic outlook to justify continued treatment. Covered therapy services shall be rehabilitative therapy services unless they meet the criteria for maintenance therapy requiring the skills of a therapist described below.
Buy tadalafil overnight. Rita Ora | Your Song (ft. Ed Sheeran).
Alternatively yellow 5 impotence order tadalafil 2.5mg fast delivery, women of child-bearing age may be immunized against tetanus with a single-antigen vaccine erectile dysfunction underwear discount tadalafil 10mg with visa. Wounds are considered to be tetanus-prone if they are sustained either more than 6 hours before surgical treatment of the wound or at any interval after injury and show one or more of the following: a puncture-type wound erectile dysfunction doctors in houston tx order discount tadalafil, a compound fracture impotence nhs buy generic tadalafil pills, a wound containing foreign bodies erectile dysfunction drugs natural discount tadalafil 2.5 mg line, a significant degree of devitalized tissue high cholesterol causes erectile dysfunction buy tadalafil 2.5mg lowest price, clinical evidence of sepsis, contamination with soil/manure likely to contain tetanus organisms. For clean wounds, fully immunized individuals (those who have received a total of 5 doses of tetanus vaccine at appropriate intervals) and those whose primary immunization is complete (with boosters up to date) do not require tetanus vaccine; individuals whose primary immunization is incomplete or whose boosters are not up to date require a reinforcing dose of tetanus vaccine (followed by further doses as required to complete the schedule); non-immunized individuals (or those whose immunization status is not known or who have been immunized but are now immunocompromised) should be given a dose of the vaccine immediately (followed by completion of the full course of the vaccine if records confirm the need). For tetanus-prone wounds, management is as for clean wounds with the addition of a dose of antitetanus immunoglobulin (section 19. Antibacterial prophylaxis (with benzylpenicillin, or amoxicillin with clavulanic acid, or metronidazole) may also be required for tetanus prone wounds (see section 6. For combined Diphtheria, pertussis and tetanus vaccine, and combined Diphtheria and tetanus vaccines, see under Diphtheria vaccine. Immunologicals Uses: active immunization against tetanus and neonatal tetanus; tetanus prophylaxis as part of wound management (tetanus-prone wounds and clean wounds). If schedule requires tetanus vaccine and antitetanus immunoglobulin to be administered at the same time, they should be administered using separate syringes and separate sites. Immunization against typhoid fever is recommended for children of school-age and adults in endemic areas, travellers to endemic areas, and laboratory workers handling specimens from suspected cases. The vaccines do not provide complete protection and should not replace hygiene precautions. Immunologicals A single dose of parenteral Vi capsular polysaccharide vaccine is recommended for adults and children over 2 years of age, followed by booster doses every 3 years in cases of continued exposure. A live oral typhoid vaccine containing an attenuated strain of Salmonella typhi (Ty21a) is available either as enteric coated capsules, or as a liquid suspension. The capsules are licensed for individuals over 5 years of age and are given as 4 doses, each 2 days apart; the suspension can be administered to children over 2 years of age and is given as 3 doses, each 2 days apart. In endemic areas, a booster dose of the live oral vaccine is recommended every 3 years; for travellers to endemic areas from non-endemic areas an annual booster is recommended. Inactivated whole-cell typhoid vaccines may still be available in some countries; children over 5 years of age are given 2 doses separated by an interval of 4 weeks, with a booster dose every 3 years. Capsule, live attenuated strain of Salmonella typhi (Ty21a) Oral suspension, live attenuated strain of Salmonella typhi (Ty21a) Injection, Vi capsular polysaccharide typhoid: 25 microgram/0. Administration of oral typhoid vaccine should be coordinated so that the antimalarial, mefloquine, is not taken for at least 12 hours before or after a dose; vaccination should be completed at least 3 days before the first dose of mefloquine or other antimalarials (except proguanil hydrochloride in combination with atovaquone, which may be given concomitantly). Oral typhoid vaccine is inactivated by concomitant administration of antibacterials; if possible antibacterials should be avoided 3 days before, or 3 days after, vaccination. Varicella vaccine Varicella-zoster (chickenpox) is a highly contagious disease caused by varicella-zoster virus. Various formulations of the live, attenuated vaccine based on the Okastrain are available. Varicella-zoster vaccine may be used as part of a national childhood immunization programme. The vaccine may also be used in adolescents or adults without a history of varicella but who are at increased risk of infection. Post-exposure vaccination can be considered for seronegative health-care workers who come into direct contact with patients with varicella-zoster. Contraindications: see introductory notes; also pregnancy (avoid pregnancy for 3 months after vaccination; Appendix 2); immunodeficiency; patients receiving immunosuppressive therapy; untreated active tuberculosis. Precautions: see introductory notes; also family history of congenital immune disorders. Immunologicals Yellow fever vaccine Yellow fever is a viral haemorrhagic fever which is endemic in tropical regions of Africa and South America. Yellow fever 17D vaccine is a live, attenuated vaccine, which offers protection from 10 days after vaccination, for at least 10 years. Yellow fever vaccine is also recommended for people at high risk of yellow fever exposure, including forestry and agricultural workers, and people living in or travelling to endemic areas. During epidemics, mass vaccination campaigns should be initiated as early as possible. Contraindications: see introductory notes; also not recommended for infants under 9 months of age. Precautions: see introductory notes; also pregnancy (Appendix 2); interactions: Appendix 1. Adverse effects: see introductory notes; also headache, myalgia, weakness; very rarely encephalitis (infants more susceptible); viscerotropic disease, multiple organ failure (the elderly more susceptible). Muscle relaxants (peripherally-acting) and cholinesterase inhibitors Muscle relaxants Muscle relaxants used in surgery are classified according to their mode of action as either depolarizing or non-depolarizing neuromuscular blocking drugs. They should never be given until it is certain that general anaesthesia has been established and ventilation must be mechanically assisted until they have been completely inactivated. It produces rapid, complete paralysis, which is very short lasting in most patients and is of particular value for laryngoscopy and intubation. Should paralysis be prolonged, ventilation must be assisted until muscle function is fully restored. Alcuronium is a non-depolarizing muscle relaxant with a duration of action of about 30 minutes. Its effects may be rapidly reversed after surgery by the anticholinesterase, neostigmine (see below), provided atropine (section 1. Cholinesterase inhibitors Reversal of block Cholinesterase inhibitors, such as neostigmine, are used at the end of an operation to reverse the muscle paralysis produced by non-depolarizing blocking drugs, such as alcuronium and vecuronium. Neostigmine must not be used with depolarizing blocking drugs, such as suxamethonium, since neostigmine will prolong the muscle paralysis. Neostigmine is also used to treat postoperative non-obstructive urinary retention. Myasthenia gravis Cholinesterase inhibitors, such as neostigmine and pyridostigmine, are used in the symptomatic treatment of myasthenia gravis. They act by inhibiting acetylcholinesterase, thereby prolonging the action of acetylcholine, and thus enhancing neuromuscular transmission; this produces at least a partial improvement in most myasthenic patients but complete restoration of muscle strength is rare. Unless the patient has difficulty in swallowing, cholinesterase inhibitors are given by mouth. Doses should be carefully adjusted to avoid precipitating a cholinergic crisis due to overdosage; this must be differentiated from a myasthenic crisis because of disease progression, and consequent underdosage; the principal effect in both cases is increased muscle weakness. In myasthenic crisis, if the patient has difficulty in breathing and in swallowing, the cholinesterase inhibitor must be given by intramuscular or subcutaneous injection; neostigmine is usually preferred over pyridostigmine in such cases. Precautions: renal impairment (Appendix 4); hepatic impairment (Appendix 5); burns patients (possibly increase dose); electrolyte disturbances; respiratory acidosis or hypokalaemia (possibly decrease dose); history of asthma; pregnancy (Appendix 2) and breastfeeding (Appendix 3); interactions: Appendix 1. Adverse effects: histamine release, leading to allergic reactions, such as wheal and flare effects at site of injection, flushing, and bronchospasm (anaphylactoid reactions reported); transient hypotension, slight increase in heart rate or decreased pulse rate. Muscle relaxants (peripherally-acting) and cholinesterase inhibitors Neostigmine Injection: 500 micrograms in 1-ml ampoule; 2. Uses: myasthenia gravis; reversal of non-depolarizing muscle relaxants administered during surgery, postoperative non-obstructive urinary retention. Contraindications: recent intestinal or bladder surgery; mechanical intestinal or urinary tract obstruction; after suxamethonium; pneumonia; peritonitis. Precautions: asthma; urinary tract infections; cardiovascular disease including arrhythmias (especially bradycardia, vagotonia, recent myocardial infarction or atrioventricular block); hyperthyroidism; hypotension; peptic ulcer; epilepsy; parkinsonism; renal impairment (Appendix 4); pregnancy (Appendix 2) and breastfeeding (Appendix 3); interactions: Appendix 1. Muscle relaxants (peripherally-acting) and cholinesterase inhibitors and micturition, miosis, nystagmus, bradycardia, heart block, arrhythmias, hypotension, agitation, excessive dreaming, and weakness eventually leading to fasciculation and paralysis; thrombophlebitis reported; rash associated tablet (bromide salt) formulations. Precautions: asthma; urinary tract infection; cardiovascular disease including arrhythmias (especially bradycardia or atrioventricular block); hyperthyroidism; hypotension; peptic ulcer; epilepsy; parkinsonism; avoid intravenous injection; renal impairment (Appendix 4); pregnancy (Appendix 2) and breastfeeding (Appendix 3); interactions: Appendix 1. Adverse effects: muscarinic effects generally weaker than those associated with neostigmine; and include increased salivation, nausea and vomiting, abdominal cramps, and diarrhoea; signs of overdosage include bronchoconstriction, increased bronchial secretions, lacrimation, excessive sweating, involuntary defecation and micturition, miosis, nystagmus, bradycardia, heart block, arrhythmias, hypotension, agitation, excessive dreaming, and weakness eventually leading to fasciculation and paralysis; thrombophlebitis; rash associated with tablet (bromide salt) formulations. Muscle relaxants (peripherally-acting) and cholinesterase inhibitors Suxamethonium Injection: 50 mg (chloride)/ml in 2-ml ampoule. Uses: brief muscular paralysis during endotracheal intubation, endoscopy and electroconvulsive therapy. Contraindications: inability to maintain clear airway; personal or family history of malignant hyperthermia; neurological disease involving acute wasting of major muscle, prolonged immobilization (risk of hyperkalaemia); personal or family history of congenital myotonic disease; Duchenne muscular dystrophy; myasthenia gravis; glaucoma, ocular surgery; liver disease; burns; low plasma cholinesterase activity (including severe liver disease); hyperkalaemia. Precautions: digitalis toxicity or recent digitalization; cardiac, respiratory or neuromuscular disease; paraplegia, spinal cord injury, or severe trauma; severe sepsis (risk of hyperkalaemia); prolonged apnoea on repeated injection (infusion preferred for long surgical procedures); hepatic impairment (Appendix 5); renal impairment (Appendix 4); pregnancy (Appendix 2) and breastfeeding (Appendix 3); children; interactions: Appendix 1. Adverse effects: postoperative muscle pain, particularly in patients ambulant after operation in females; myoglobinuria; myoglobinaemia; prolonged apnoea; increased intraocular pressure; hyperkalaemia; bradycardia, hypotension, and arrhythmias, particularly with halothane (but, with repeated doses, tachycardia, and hypertension); increased salivary, bronchial and gastric secretions; transient rise in intragastric pressure; hypersensitivity reactions including flushing, rash, urticaria, bronchospasm, and shock (more common in women, in history of allergy, or in asthmatics); rarely malignant hyperthermia (but often fatal). Muscle relaxants (peripherally-acting) and cholinesterase inhibitors Vecuronium Powder for injection: 10 mg (bromide) in vial. Contraindications: respiratory insufficiency or pulmonary disease; dehydrated or severely ill patients; myasthenia gravis or other neuromuscular disorders. Precautions: hepatic impairment (Appendix 5); burns patients (possibly increase dose); electrolyte disturbances; respiratory acidosis or hypokalaemia (possibly decrease dose); history of asthma; severe obesity (may require maintenance of adequate airway and ventilation support); pregnancy (Appendix 2) and breastfeeding (Appendix 3); interactions: Appendix 1. To avoid excessive dosage in obese patients, dose should be calculated on the basis of ideal body weight. Adverse effects: minimal release of histamine; rarely hypersensitivity reactions including bronchospasm, hypotension, tachycardia, oedema, erythema, and pruritus). Ophthalmological preparations Administration of eye preparations Preparations for use in the eye should be sterile when issued. Use of single application containers is preferable; multiple-application preparations include the antimicrobial preservatives and when used particular care should be taken to prevent contamination of the contents, for example, by avoiding contact between the applicator and the eye or other surfaces. Eye drops are generally instilled into the lower conjunctival sac which is accessed by gently pulling down the lower eyelid to form a pocket into which one drop is instilled. A small amount of eye ointment is applied similarly; the ointment melts rapidly and blinking helps to spread it. When two different eye drops are required at the same time, dilution and overflow may occur if one immediately follows the other; an interval of at least five minutes should therefore be allowed between the two applications. Systemic absorption, which may occur after topical application of eye drops, can be minimized by using the finger to compress the lacrimal sac at the medial canthus for at least one minute after instillation of the drops. Performance of skilled tasks Application of eye preparations may cause blurring of vision which is generally transient; patients should be advised not to carry out skilled tasks, such as operating machinery or driving, until their vision has cleared. However, in some cases, for example, in gonococcal conjunctivitis, both topical and systemic anti-infective treatment may be necessary. Blepharitis and conjunctivitis are often caused by staphylococcus, while keratitis and endophthalmitis may be bacterial, viral, or fungal. Although most cases of acute bacterial conjunctivitis may resolve spontaneously, anti-infective treatment shortens the infectious process and prevents complications. Acute infective conjunctivitis is treated with antibacterial eye drops by day and eye ointment applied at night. Ophthalmological preparations Aciclovir is an antiviral used in the treatment of keratitis due to herpes simplex virus. Gentamicin is a broad-spectrum bactericidal aminoglycoside antibiotic with particular activity against Pseudomonas aeruginosa, Neisseria gonorrhoea and other bacteria that may be implicated in blepharitis or conjunctivitis. Tetracycline is a broad spectrum antibiotic with activity against many Gram positive and Gram-negative bacteria including N. Ophthalmic tetracycline is used in blepharitis, conjunctivitis, and keratitis produced by susceptible bacteria. Tetracycline is also used in the treatment of trachoma caused by Chlamydia trachomatis and in the prophylaxis of neonatal conjunctivitis (ophthalmia neonatorum) caused by N. Uses: keratitis caused by herpes simplex; systemic herpes simplex infections (section 6. Adverse effects: local irritation including transient mild stinging, inflammation; superficial punctuate keratopathy reported; very rarely hypersensitivity reactions including angioedema. Uses: blepharitis; bacterial conjunctivitis; systemic bacterial infections (section 6. Contraindications: hypersensitivity to aminoglycoside group of antibiotics Precautions: prolonged use may lead to skin sensitization and emergence of resistant organisms including fungi; discontinue if there is purulent discharge, inflammation or exacerbation of pain. Uses: superficial bacterial infection of the eye; mass treatment of trachoma in endemic areas; prophylaxis of neonatal conjunctivitis (ophthalmia neonatorum) due to Neisseria gonorrhoea or Chlamydia trachomatis. Anti-inflammatory agents Ophthalmic corticosteroids should only be used under supervision of an ophthalmologist as inappropriate use is potentially blinding. Dangers include the development of open-angle glaucoma (chronic simple glaucoma) and cataracts, and the aggravation of a simple herpes simplex epithelial lesions into extensive corneal ulcers and subsequent permanent corneal scarring, with possible damage to vision and even loss of the eye. Corticosteroids such as prednisolone are useful in the treatment of inflammatory eye conditions including uveitis and scleritis.
Liebmann J erectile dysfunction and diabetes medications purchase 10mg tadalafil fast delivery, Ritch R: Familial congenital cataracts and iris colobomas erectile dysfunction operations discount tadalafil 20 mg amex, Ophthalmic Genetics Study Club impotence of proofreading poem buy cheap tadalafil 2.5 mg on-line, Dallas new erectile dysfunction drugs 2012 tadalafil 2.5mg with amex, Texas erectile dysfunction pump on nhs purchase tadalafil overnight delivery, Nov 7 impotence restriction rings cheap tadalafil 5mg visa, l987 75. Rubio M, Ritch R, Steinberger D: National Exhibit of Blind Artists, Am Acad Ophthalmol, Dallas, Nov 8-l3, l987 78. Ritch R: Factors in the success of argon laser trabeculoplasty, European Ophthalmologic Congress, Lisbon, Portugal, May 19, 1988 86. Ritch R: Glaucoma surgery in pseudophakia, European Congress of Ophthalmology, Brussels, Belgium, Sept 16, 1988 87. Ritch R: Classification of angle-closure glaucoma, Canadian Ophthalmol Soc, Toronto, Ont, Sept 23, 1988 88. Ritch R: Pigmentary dispersion syndrome, Canadian Ophth Soc, Toronto, Ont, Sept 23, 1988 89. DiSclafani M, Liebmann J, Ritch R: Pigmentary dispersion syndrome and myopia: Hereditary aspects, Ophthalmic Genetics Discussion Club, Las Vegas, Oct 8, 1988. Fiero R, Ritch R, Steinberger D: Altered cognitive function caused by carbonic anhydrase inhibitors. Teekhasaenee C, Ritch R, Rutnin U, Leelawongs N: Glaucoma in oculodermal melanocytosis. Ritch R: Glaucoma and uveitis, Intl Ophthalmology Congress, Singapore, March 20, 1990. Liebmann J, Ritch R, Pollack I, Robin A, Harrison R, Levene R: Argon laser trabeculoplasty in pigmentary glaucoma: long-term follow-up. Kupersmith M, Ritch R: Non-glaucomatous optic neuropathy does not predispose to glaucomatous damage from elevated intraocular pressure. Wolner B, Liebmann J, Ritch R: Late bleb-related endophthalmitis after trabeculectomy with adjunctive 5 fluorouracil. Buxton J, Lavery K, Liebmann J, Buxton B, Ritch R: Reconstruction of filtering blebs with free conjunctival autografts. Greenstein V, Shapiro A, Carr R, Haroomi M, Hood D, Ritch R, Zaidi O: Chromatic and achromatic threshold changes associated with ocular disorders. Ritch R, Hu Dan-Ning: Human iris pigment epithelium in culture; methods of isolation, growth patterns, and morphology in vitro. Liebmann J, Weseley P, Walsh J, Ritch R, Marmor M: Pigment dispersion syndrome and lattice degeneration of the retina. Pelton-Henrion K, Hu D-N, Ritch R, McCormick S: Human uveal melanocytes: novel isolation and propagation techniques for adult human cell cultures. Scharf B, Chi T, Grayson D, Ritch R, Liebmann J: Argon laser trabeculoplasty for angle-recession glaucoma. Pape L, Ritch R, Liebmann J, Steinberger D: Long-term compassionate use of apraclonidine 0. Chi T, Grayson D, Scharf B, Liebmann J, Ritch R: Ab interno filtration using an automated trephine. Greenstein V, Ritch R, Shapiro A, Zaidi O, Hood D: the effects of glaucoma on cone pathways. Teekhasaenee C, Wutthipan S, Ritch R: Combined oculodermal melanocytosis and Klippel-Trenaunay Weber Syndrome with congenital glaucoma. High resolution ultrasound biomicroscopy of the anterior segment in patients with dense corneal scars. High frequency ultrasound biomicrosopy of the anterior segment following intraocular lens implantation. High frequency ultrasound biomicroscopic imaging of complications after cataract surgery. Reproducibility of measurement of anterior segment parameters by high resolution ultrasound biomicroscopy. Biometric measurement of anterior chamber depth in pseudophakes using high resolution ultrasound biomicroscopy. Prevalence of narrow angles and angle-closure in populations undergoing glaucoma screening. The effect of brimonidine tartrate in glaucoma patients on maximal medical therapy. Goldenfeld M, Wong P, Ruderman J, Rosenberg L, Krupin T, Geiser D, Liebmann J, Ritch R. Ultrasound biomicroscopy before and after laser iridectomy in pigmentary glaucoma. The effect of brimonidine tartrate in glaucoma patients on maximum medical therapy. Ritch R: Anterior segment ultrasound biomicroscopy in the diagnosis and treatment of glaucoma. Blinking indents the cornea and reduces anterior chamber volume as shown by ultrasound biomicroscopy. Robin A, Ritch R, Shin D, Smythe B, McCarty G, Taylor B, Silver L, DeFaller J, Godio L. Delay of surgery by apraclonidine in patients on maximally tolerated medical therapy for glaucoma. Ciliary body enlargement in Sturge-Weber syndrome (Encephalotrigeminal angiomatosis). Glaucoma Committee of the International Congress, Quebec, Canada, June 23-24, 1994. International Congress of Ophthalmology Video Presentation, Toronto, Ontario, June 26-30, 1994. Camras C, Wax M, Ritch R et al: Latanoprost: A potent ocular hypotensive prostaglandin analog, increases pigmentation in peripherally hypopigmented irides. Horwitz B, Stewart W, Ritch R, Laibovitz R, Stewart R, Kottler M: A double-masked, 90 day study of the efficacy of 0. The short term efficacy of apraclonidine hydrochloride when added to maximum tolerated medical therapy. Discussion of Kuchle M: Incidence of secondary cataract in pseudoexfoliation syndrome. Ishikawa H, Liebmann J, Uji Y, Ritch R: A new method of color mapping the anterior chamber angle with ultrasound biomicroscopy. Gramer E, Thiele H, Ritch R: Genetic predisposition to pigment dispersion syndrome and pigmentary glaucoma. N: neuroprotective effect of various factors on cultured adult human retinal ganglion cells. Ritch R: Discussion of Pillunat, L: Ultrasound biomicroscopy of pigment dispersion syndrome. Ritch R: New approaches to the treatment of glaucoma, 75th Anniversary Symposium of the Brazilian Ophthalmologic Society, Rio de Janeiro, Brazil, Nov 28, 1997. Quantitative evaluation of intraretinal reflectivity with optical coherence tomography. Agreement between scanning laser polarimetry and achromatic automated perimetry using a neural network. Factors associated with baseline intraocular pressure variability in the Collaborative Initial Glaucoma Treatment Study. Increasing sampling density improves optical coherence tomography measurement reliability. Reflectivity vs retardation: optical coherence tomography and scanning laser polarimetry. Glaucoma Committee of the International Congress, Edinburgh, Scotland, June 15, 1998. Glaucoma Committee of the International Congress, Edinburgh, Scotland, June 16, 1998. Analysis of Myocilin Mutations in 1800 Glaucoma Patients from Five Different Populations. Discussion of Kuchle M, et al: Anterior chamber depth and complications during cataract surgery in pseudoexfoliation syndrome. Williams M, Ritch R: Understanding cultural differences in international teleophthalmology consultations (poster). Chen H, Greenstein V, Seiple W, Park R, Ritch R: Does pigment dispersion syndrome affect retinal pigment epithelial function Ritch R: Management of angle-closure glaucoma when intraocular pressure is not controlled by laser iridotomy. Ritch R: Discussion of Glovinsky Y, Levy Y: Red and blond hair is associated with pigmentary glaucoma. Ritch R: Discussion of Haargaard B, et al: Exercise and iris bowing in healthy eyes. Ritch R: Discussion of Quaranta et al: the effect of Ginkgo biloba extract on visual field damage in normal tension glaucoma. Nineteenth Singapore Malaysia Ophthalmological Conference, Penang, Malaysia, June 2001. Invest Ophthalmol Vis Sci 2002:42(Suppl) Also presented at the American Medical Students Association, 401. Albekioni Z, Joson P, Tello C, Liebmann J, Ritch R: Correlation between central corneal thickness and scleral thickness. Glaucoma Society of the International Congress of Ophthalmology, Chantilly, France, May 30, 2003. Shildkrot Y, Liebmann J, Fabijanczyk B, Tello C, Ritch R: Central corneal thickness variability over time in normal and glaucomatous eyes. Tello C, Oliveira C, Liebmann J, Ritch R: Does ciliary body thickness correlate with refractive error and axial length Ritch R: Indications for argon laser peripheral iridoplasty after laser peripheral iridotomy. Ritterband D, Shapiro D, Trubnik V, Meskin S, Seedor J, Koplin R, Shabto U, Liebmann J, Tello C, Ritch R: Long-term results of penetrating keratoplasty with simultaneous pars plana glaucoma drainage implants. Seedor J, Ritterband D, Trubnik V, Meskin S, Seedor J, Koplin R, Shabto U, Liebmann J, Tello C, Ritch R: Acute post-operative complications following simultaneous penetrating keratoplasty and glaucoma drainage implant insertion. Tello C, Shihadeh W, Grippo T, Schargus M, Gramer E, Liebmann J, Ritch R: Optic Nerve Head Drusen and Visual Field Loss in Normotensive and Hypertensive Eyes. Rezaie T, Child A, Popinchalk S, Krupin T, Ritch R, Liebmann J, Ilitchev E, Crick R, Sarfarazi M: Large Scale Sequencing of the Optineurin Gene in Familial and Sporadic Cases With Primary Open-Angle Glaucoma. Schargus M, Grippo T, Ritch R, Gramer E: Stage of Visual Field Loss in Relation to the Appearance of the Optic Disc in 144 Eyes of Patients With Drusen of the Optic Disc. Teekhasaenee C, Ritch R: Goniosynechialysis following unsuccessful phacoemulsification in residual synechial angle-closure glaucoma. Ritch R: Angle-closure: A century of controversy, nonbelievers, missed opportunities, and reinventing wheels. Sirampuj P, Teekhasaenee C, Ritch R: Inferior posterior lip sclerectomy and anterior chamber inflation for uncontrolled total hyphema. Teekhasaenee C, Ritch R: Long-term follow-up of combined phacoemulsification and goniosynechialysis for uncontrolled angle-closure. Ritch R: Exfoliation syndrome and pigment dispersion syndrome: Paradigm of an overlap syndrome. Dorairaj S, Ritch R: Prevalence of monocular childhood blindness in a rural population of southern India (poster). Hsu W-C, Ritch R, Krupin T, Chen H-L: Tissue bioengineering for bleb defects: an animal study. International Glaucoma Risk and Disease Management Symposium, Toronto, Ont, Canada, Oct 18, 2008. Ritch R, Atherton S: International Teaching Consortium: Mission to Kazakhstan, 2006. The short-term effect of trabeculectomy on the intraocular pressure of the contralateral eye. Macular Changes Detected by Fourier Domain Optical Coherence Tomography in Patients with Hypotony Without Clinical Maculopathy. Ritch R: Translating research in optic nerve protection and regeneration into therapy. Anand A, etc: Lower corneal hysteresis predicts laterality in asymmetric open-angle glaucoma. Association for Research in Vision and Ophthalmology, Fort Lauderdale, May 5, 2010. A randomized trial of brimonidine versus timolol in preserving visual function: results from the Low-pressure Glaucoma Treatment Study. Treatment of exfoliative glaucoma and its potential prevention, Nadi al Bassar Congress, Tunis, Tunisia, June 4, 2011. Charimet Kanchararanya Memorial Lecture, Fifth Annual Bangkok Ophthalmologic Congress Bangkok, Thailand, Jan 5, 1989. The Schlaegel Lecture, Univ Indiana School of Medicine, Indianapolis, Indiana, Sept. Ticho Lecture, International Glaucoma Congress, Jerusalem, Israel, March 16, 1998. King Khaled Memorial Lecture, Scientific meeting of the Saudi Ophthalmological Society, Riyadh, Saudi Arabia, March 4, 2003. Prevention of Blindness Shield Lecture, Saudi Ophthalmological Society, Riyadh, Saudi Arabia, March 1, 2010. Philippine Acad Ophthalmol, Philippine Gen Hosp, Manila, Philippines, July 5, 1982 68.