Robert Forman, MD
- Department of Medicine
- Division of Cardiology
- Albert Einstein College of Medicine
- Montefiore Medical Center
- Bronx, NY
The diagnosis of pneumonia may be missed because the classic symptoms of cough erectile dysfunction pump australia order super avana 160mg with mastercard, chest pain erectile dysfunction statistics uk buy super avana with a visa, sputum production blood pressure drugs erectile dysfunction order super avana paypal, and fever may be absent or masked in elderly patients impotence after 60 160mg super avana mastercard. Abnormal breath sounds erectile dysfunction cream super avana 160 mg cheap, for example erectile dysfunction natural remedies diabetes order super avana with a visa, may be caused by microatelectasis that occurs as a result of decreased mobility, decreased lung volumes, or other respiratory function changes. Supportive treatment includes hydration (with caution and with frequent assessment because of the risk of fluid overload in the elderly); supplemental oxygen therapy; and assistance with deep breathing, coughing, frequent position changes, and Pneumonia 553 early ambulation. To reduce or prevent serious complications of pneumonia in the elderly, vaccination against pneumococ cal and influenza infections is recommended. Medical Management • Antibiotics are prescribed on the basis of Gram stain results and antibiotic guidelines (resistance patterns, risk factors, etiology must be considered. Nursing Interventions Improving Airway Patency • Encourage hydration: fluid intake (2 to 3 L/day) to loosen secretions. Promoting Rest and Conserving Energy • Encourage the debilitated patient to rest and avoid overexertion and possible exacerbation of symptoms. Promoting Fluid Intake and Maintaining Nutrition • Encourage fluids (2 L/day minimum with electrolytes and calories. Promoting Patients Knowledge • Instruct on cause of pneumonia, management of symptoms, signs and symptoms that should be reported to the physician or nurse, and the need for follow-up. Monitoring and Preventing Potential Complications • Monitoring for continuing symptoms of pneumonia (patients usually begin to respond to treatment within 24 to 48 hours after antibiotic therapy is initiated. Pneumothorax and Hemothorax P Pneumothorax occurs when the parietal or visceral pleura is breached and the pleural space is exposed to positive atmos pheric pressure. Normally the pressure in the pleural space is negative or subatmospheric; this negative pressure is required to maintain lung inflation. When either pleura is breached, air enters the pleural space, and the lung or a por tion of it collapses. Hemothorax is the collection of blood in the chest cavity because of torn intercostal vessels or lac eration of the lungs injured through trauma. Types of Pneumothorax Simple Pneumothorax A simple, or spontaneous, pneumothorax occurs when air enters the pleural space through a breach of either the parietal Pneumothorax and Hemothorax 557 or visceral pleura. Most commonly this occurs as air enters the pleural space through the rupture of a bleb or a bronchopleural fistula. A spontaneous pneumothorax may occur in an appar ently healthy person in the absence of trauma due to rupture of an air-filled bleb, or blister, on the surface of the lung, allowing air from the airways to enter the pleural cavity. Traumatic Pneumothorax A traumatic pneumothorax occurs when air escapes from a laceration in the lung itself and enters the pleural space or from a wound in the chest wall. It may result from blunt trauma (eg, rib fractures), penetrating chest or abdominal trauma (eg, stab wounds or gunshot wounds), or diaphrag matic tears. Traumatic pneumothorax may occur during inva sive thoracic procedures (ie, thoracentesis, transbronchial lung biopsy, insertion of a subclavian line) in which the pleura is inadvertently punctured, or with barotrauma from mechanical ventilation. A traumatic pneumothorax resulting from major injury to the chest is often accompanied by hemothorax. It occurs when a wound in the chest wall is large enough to allow air to pass freely in and out of the thoracic cavity with P each attempted respiration. Stopping the flow of air through the opening in the chest wall is a life-saving measure. Tension Pneumothorax A tension pneumothorax occurs when air is drawn into the pleural space and is trapped with each breath. Mediastinal shift (shift of the heart and great vessels and trachea toward the unaffected side of the chest) is a life-threatening medical emergency. The clinical picture is one of air hunger, agitation, increas ing hypoxemia, central cyanosis, hypotension, tachycardia, and profuse diaphoresis. Medical Management P the goal is evacuation of air or blood from the pleural space. A chest tube is then inserted and connected to suction to remove the remaining air and fluid, reestablish the neg ative pressure, and reexpand the lung. Nursing Management • Promote early detection through assessment and identifica tion of high-risk population; report symptoms. If the cause cannot be corrected, phlebotomy may be necessary to reduce hypervolemia and hyperviscosity. Polycythemia Vera (Primary) Polycythemia vera, or primary polycythemia, is a proliferative disorder a proliferative disorder of the myeloid stem cells. The bone marrow is hypercellular, and the erythrocyte, leukocyte, and platelet counts in the peripheral blood are elevated. Diagnosis is based on an elevated erythrocyte mass, a normal oxygen saturation level, and often an enlarged spleen. The erythropoietin level may not be as low as would be expected with an elevated hematocrit. Clinical Manifestations Patients typically have a ruddy complexion and splenomegaly. P the symptoms are due to the increased blood volume (headache, dizziness, tinnitus, fatigue, paresthesias, and blurred vision) or to increased blood viscosity (angina, claudication, dyspnea, and thrombophlebitis. Blood pressure and uric acid are often elevated, and pruritus is another common and both ersome complication. Medical Management the objective of management is to reduce the high red blood cell mass. Prostatitis 561 • Anagrelide (Agrylin) may be used to inhibit platelet aggrega tion and control the thrombocytosis related to polycythemia. Nursing Management • Assess risk factors for thrombotic complications and teach patient to recognize signs and symptoms of thrombosis. Prostatitis Prostatitis is an inflammation of the prostate gland that is often associated with lower urinary tract symptoms and symp toms of sexual discomfort and dysfunction. Prostatitis may be caused by infectious agents (bacteria, fungi, mycoplasma) or other conditions (eg, urethral stricture, benign prostatic hyperplasia. Specific treatment is based on the type of prostatitis and on the results of culture and sensitivity testing of the urine. Pruritus 563 • Encourage fluids to satisfy thirst but do not force them, because effective drug levels must be maintained in urine. Scratching the itchy area causes the inflamed cells and nerve endings to release histamine, which pro P duces more pruritus and, in turn, a vicious itch–scratch cycle. Scratching can result in altered skin integrity with excoriation, redness, raised areas (wheals), infection, or changes in pigmentation. Although pruritus usually is due to primary skin disease, it may also reflect systemic internal disease, such as diabetes mellitus; renal, hepatic, thyroid, or blood disorders; or cancer. Pruritus may be caused by cer tain oral medications (aspirin, antibiotics, hormones, opi oids), contact with irritating agents (soaps, chemicals), or prickly heat (miliaria. It may also be a side effect of radi ation therapy, a reaction to chemotherapy, or a symptom of infection. Cold compresses, ice cubes, or cool agents that contain sooth ing menthol and camphor may be applied. Psoriasis 565 • When the underlying cause of pruritus is unknown and fur ther testing is required, explain each test and the expected outcome. Psoriasis Psoriasis is a chronic, noninfectious, inflammatory disease of the skin in which the production of epidermal cells occurs faster than normal. Onset may occur at any age but is most common between the ages of 15 and 35 years. Main sites of the body affected are the scalp, areas over the elbows and knees, lower part of the back, and genitalia, as well as the nails. Psoriasis may be associ ated with asymmetric rheumatoid factor–negative arthritis of multiple joints. An exfoliative psoriatic state may develop in which the disease progresses to involve the total body surface (erythrodermic psoriatic state. Pathophysiology the basal skin cells divide too quickly, and the newly formed P cells become evident as profuse scales or plaques of epidermal tissue. As a result of the increased number of basal cells and rapid cell passage, the normal events of cell maturation and growth cannot occur, which prevents the normal protective layers of the skin to form. Periods of emotional stress and anxiety aggravate the con dition, and trauma, infections, and seasonal and hormonal changes also are trigger factors. Clinical Manifestations Symptoms range from a cosmetic annoyance to a physically disabling and disfiguring affliction. Psychological Considerations • Psoriasis may cause despair and frustration; observers may stare, comment, ask embarrassing questions, or even avoid the person. Assessment and Diagnostic Methods • Presence of classic plaque-type lesions (change histologically progressing from early to chronic plaques) • Signs of nail and scalp involvement and positive family history P Medical Management Goals of management are to slow the rapid turnover of epi dermis, to promote resolution of the psoriatic lesions, and to control the natural cycles of the disease. The therapeutic approach should be under standable, cosmetically acceptable, and not too disruptive of lifestyle. An assessment is made of lifestyle, because psoriasis is signif icantly affected by stress. The most important principle of pso riasis treatment is gentle removal of scales (bath oils, coal tar preparations, and a soft brush used to scrub the psoriatic plaques. After bathing, the application of emollient creams containing alpha-hydroxy acids (Lac-Hydrin, Penederm) or salicylic acid will continue to soften thick scales. Psoriasis 567 Topical Therapy • Topical treatment is used to slow the overactive epidermis. Calcipotriene (Dovonex; not recommended for use by elderly patients because of their more fragile skin, or in pregnant or lactating women); and tazarotene (Tazorac) as well as vitamin D are additional nonsteroidal agents. Medica tions may be in the form of lotions, ointments, pastes, creams, and shampoos. Systemic Therapy • Biologic agents act by inhibiting activation and migration, eliminating the T cells completely, slowing postsecretory cytokines or inducing immune deviation: infliximab (Rem icade), etanercept (Enbrel), efalizumab (Raptiva), ale P facept (Amevive), and adalimumab (Humira. Biological agents have significant side effects, making close monitor ing essential. Nursing Management Assessment Assessment focuses on how the patient is coping with the skin condition, the appearance of normal skin, and the appear ance of skin lesions. Nursing Interventions P Promoting Understanding • Explain with sensitivity that there is no cure and that life time management is necessary; the disease process can usu ally be controlled. Psoriasis 569 • Inform patient that water should not be too hot and skin should be dried by patting with a towel. Improving Self-Concept and Body Image Introduce coping strategies and suggestions for reducing or coping with stressful situations to facilitate a more positive outlook and acceptance of the disease. Monitoring and Managing Complications • Psoriatic arthritis: Note joint discomfort and evaluate fur ther. Promoting Home and Community-Based Care Teaching Patients Self-Care • Advise patient that topical corticosteroid preparations on face and around eyes predispose to cataract development. With increased resistance to left ventricular filling, blood backs up into the pulmonary circulation. The patient quickly develops pulmonary edema, sometimes called flash pulmonary edema, from the blood volume overload in the lungs. Pulmonary edema can also be caused by noncardiac disorders, such as renal failure and other conditions that cause the body to retain fluid. The rapid increase in atrial pressure results in an acute increase in pulmonary venous pressure, which produces an increase in hydrostatic pressure that forces fluid out of the pul monary capillaries into the interstitial spaces and alveoli. Clinical Manifestations • As a result of decreased cerebral oxygenation, the patient becomes increasingly restless and anxious. Along with a sudden onset of breathlessness and a sense of suffocation, the patients hands become cold and moist, the nail beds become cyanotic (bluish), and the skin turns ashen (gray. Pulmonary Edema, Acute 571 Assessment and Diagnostic Methods • Diagnosis is made by evaluating the clinical manifestations resulting from pulmonary congestion. Medical Management Goals of medical management are to reduce volume overload, improve ventricular function, and increase respiratory exchange using a combination of oxygen and medication therapies. Observe patient for exces sive respiratory depression, hypotension, and vomiting. Clinical Manifestations Symptoms depend on the size of the thrombus and the area of the pulmonary artery occlusion. Pulmonary Embolism 573 • Chest pain is common, usually sudden in onset and pleu ritic in nature; it can be substernal and may mimic angina pectoris or a myocardial infarction. Prevention P • Ambulation or leg exercises in patients on bed rest • Application of sequential compression devices • Anticoagulant therapy for patients whose hemostasis is ade quate and who are undergoing major elective abdominal or thoracic surgery Medical Management Immediate objective is to stabilize the cardiopulmonary system. P • Patients must continue to take some form of anticoagula tion for at least 3 to 6 months after the embolic event. Other side effects include fever, abnormal liver function, and allergic skin reaction. Thrombolytic Therapy • Thrombolytic therapy may include urokinase, streptokinase, and alteplase. Preventing Thrombus Formation • Encourage early ambulation and active and passive leg exer cises. Monitoring Anticoagulant and Thrombolytic Therapy • Advise bed rest, monitor vital signs every 2 hours, and limit P invasive procedures. Minimizing Chest Pain, Pleuritic • Place patient in semi-Fowlers position; turn and reposition frequently. Managing Oxygen Therapy • Assess the patient frequently for signs of hypoxemia and monitors the pulse oximetry values. Providing Postoperative Nursing Care • Measure pulmonary arterial pressure and urinary output. Promoting Home and Community-Based Care Teaching Patients Self-Care • Before discharge and at follow-up clinic or home visits, teach patient how to prevent recurrence and which signs and symptoms should alert patient to seek medical attention. Advise patient to use a toothbrush with soft bristles to pre vent gingival bleeding. Pulmonary Heart Disease (Cor Pulmonale) 577 • Instruct patient to avoid laxatives, which affect vitamin K absorption (vitamin K promotes coagulation. Other causes P are conditions that restrict or compromise ventilatory func tion, leading to hypoxemia or acidosis (eg, deformities of the thoracic cage, massive obesity) and conditions that reduce the pulmonary vascular bed (eg, primary idiopathic pulmonary arterial hypertension, pulmonary embolus. Certain disorders of the nervous system, respiratory muscles, chest wall, and pul monary arterial tree also may be responsible for cor pulmonale.
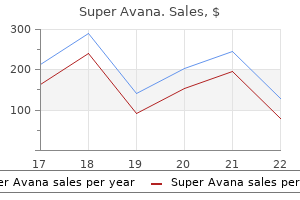
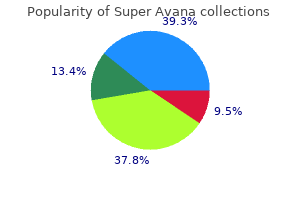
Twenty-year outcomes after breast-conserving surgery and definitive radiotherapy for mammographically detected ductal carcinoma in situ erectile dysfunction zyprexa generic 160mg super avana mastercard. Submitted 153 Chapter 7 Abstract Background: the popularity of Autologous-Fat-Transfer causes an up-rise in sophisticated scientific research and clinical implementation erectile dysfunction free samples buy super avana 160 mg mastercard. While results from the former are well-documented impotence thesaurus order super avana once a day, important aspects of the latter are less recog nized osbon erectile dysfunction pump safe 160 mg super avana. The aim of this study is to ventilate the experience of European surgeons and highlight differences between countries and level of experience erectile dysfunction drugs pictures best order for super avana. Differences between countries and level of experi ence were analyzed using a logistic-regression model erectile dysfunction drugs not working buy super avana 160mg visa. Results: the mean respondent age, out of 358 completed questionnaires, was 46 years. The thigh and abdomen were less favored harvest-locations by the Belgium and French respondents respectively and both the French and Aus trian respondents preferred manual-aspiration over liposuction in harvesting the fat. Despite minor differences between countries and experience the intra glandular space was injected in all subgroups. Discussion: Despite an obvious adherence to Coleman?s Method in Europe, deviations thereof become more apparent. Guidelines aid clinical practice and cause reproducibility but adherence regarding important aspects like injection planes deviate into possible risky territory. Whether used as permanent filler in facial reju 1,2 venation or as a volume enhancing technique in addition to onco-plastic or cosmetic surgery of the breast, much is written regarding efficacy and safety as 3-5 well as various techniques and satisfaction. Vice-versa, this acceptance leads to more and better research cur 6 rently being conducted. However, this same advantage could not be found in experimental animal and in vitro studies. Satisfaction rates among patients and surgeons are 8-11 generally assessed with the use of likert-scales or validated questionnaires 12 like the breast-Q. One way to narrow the gap between the laboratory and clinical practice is by way of professional survey studies. The national plastic surgery associations of ten European coun tries (Netherlands, Belgium, Germany, Great-Britain, France, Spain, Italy, Greece, Austria, and Switzerland) were contacted through email and, after introduction, asked for their participation in distributing this questionnaire amongst their members (active participation. When no reply was received, the organization was contacted on two additional occasions with a minimum of a 2 week interval by telephone during which the method and purpose of the study was explained and the organization was again asked for their participation in the study. Partici pating organizations distributed the questionnaire amongst its members with a reminder email following after 2-4 weeks. The questionnaire was constructed in Sur veyGizmo, an online digital survey tool and translated in the following languages; Dutch, German, Spanish, Italian and French by either a native speaking colleague or an internet-based translational service (www. A free text section was provided at the bottom of the appropriate questions to allow respondents to add personal comments. The completion of the ques tionnaire was strictly voluntary and without compensation. With this, a sample size of 350 is adequate to achieve a confidence level of 95% 158 Plastic/ Breast Surgeons on the use of/ and opinion towards Autologous Fat Transfer 22 with a margin error or confidence interval T5% for the entire population. Differences between baseline characteris tics of the respondents from different countries were assessed using t-tests for continuous variables (age) and the KruskalWallis test for ordinal variables (number of years of experience and number of procedures performed per year. Differ ences between both technical choices and attitude towards fat grafting were as sessed in relation to country, years of experience (resident, 0-10, 10-20 and >20 years of experience) and number of procedures performed per year (0-10, 10-20, >30 procedures performed per year. We used logistic regression in case of a binary response variable, ordinal regression in case of an ordinal response variable and multinomial logistic regression in case of multiple response categories. Contacted National Plastic Surgery Association Active or Passive Number of emails Response Countries participation send per country rate the Netherlands Netherlands Society for Plastic Active 425 33. A total of 358 completed questionnaires were retrieved for analysis over a 10 month peri od (June 2016 April 2017. Eighty percent were consultants, with a majority having more than 20 years of practicing experience. Table 2: Baseline Characteristics Question/ Variable Outcome: mean (%) Missing (%) Age 46 ?10. Seventy-five percent of respondents used a cannula to re-inject the fat, aiming at 1-2 cc (30. In breast-surgery, more than half (52%) of the respondents grafted the subcutaneous plane in addition to both flap and implant reconstructions as well as the correction of local defects. For flap reconstructions other planes most commonly grafted were the subglandular (31. There was a clear division in the opinion about causative factors when it comes to volume retention with approximately half of respondents attributing the results to fat-survival (50%) or a combination of fat survival and scar-tissue replacement (41. Table 5a: Differences between countries Netherlands Belgium France Austria Other (baseline) 1 No. Discrepan cies between differences between percentages and the direction of the arrows are due to correction for other variables in the model. The mean age of the Dutch respondents was significantly lower than that of other countries. Considering, harvest-locations, the thigh was significantly less used in Belgium and in the other countries combined and French respondents were less inclined to use the abdomen compared to the Dutch. The French and Aus trian respondents seemed to prefer manual-aspiration over a liposuction-device and larger over smaller cannula-sizes (>3 vs <2 mm) compared to the Dutch respondents. Furthermore, centrifugation was performed significantly more by the French and both centrifugation as well as washing significantly less by the Austrian surgeons, respectively. On the contrary, in ad dition to flap (breast) reconstructions, the French, performed significantly more sub-pectoral fat injections. Finally, when asked about the amount of injected fat both the French and the Belgian surgeons injected significantly more in addition to flap-reconstruction than the Dutch surgeons. What stands out is both the harvesting-location as well as technique and ?cannula-size, besides the estimat ed injected volume. The obvious attraction of the technique for both pa tients and surgeons comes forth from the desire to recycle fat tissue for a bene ficial often defect occupying goal in reconstructive or augmentational sur gery. Hence, the high surgeon and patient satisfaction rates that are generally 23,24 reported in clinical studies and systematic reviews. Despite an adequate overall response-rate we found a low response-rate per country which may have been attributable to the headline of the survey invita tion. More than a quarter of the respondents had >20 years of practicing experience and higher rates of these more experienced surgeons were found in all of the other coun tries compared with the Netherlands. This was probably attributable to the higher number of residents amongst the Dutch respondents. These findings are in line with Kaufman et 16 al and although a longer learning curve might be the result of the relative few procedures performed, most surgeons considered themselves experienced. The French and the Austrian respondents 168 Plastic/ Breast Surgeons on the use of/ and opinion towards Autologous Fat Transfer used a liposuction-device significantly less often than the Dutch population, which we hypothesized as possibly due to the higher level of experience (and Coleman Technique adherence) of respondents from these countries. While randomized-controlled-trials comparing both methods are clearly needed, the 27 recent systematic review by Shim et al. The preferred cannula-size when using a liposuction-device was 3mm in 41%, with an equal percentage of respondents indicating not knowing the cannula size when using manual-aspiration. This seems to be an area where improve ment can be achieved, since several studies have indicated that the size of both the aspiration and injection-cannula (>3mm < 6mm) matter significantly in 32,33 terms of adipocyte-viability. Finally, in terms of injection-technique and planes, half of the respondents aimed at injecting <1 to 2cc of fat, while over correcting 10-30% in-line with the Coleman-Method, with only the French in jecting more. What is interesting to see is that the intra-glandular plane was grafted for all indications ranging from 18. The perception of what causes the eventual volume-retention was either fat-survival or a combination thereof with scar tissue formation, and further histological animal-studies, preferably with long-term follow-up are 169 Chapter 7 needed to substantiate the answer to this question. Figure 2 highlights the order in which these concerns troubled the respondents, illustrating that further studies should focus on the oncological and radiological-safety of the technique. While the authors trust the intentions of the respondents, the accuracy of the answers given can on a subconscious level be colored by embarrassment, 39 lack-of-memory, alacrity or even boredom. Furthermore, discrepancy between responders and non-responders can create a selection bias. Finally, while the questions leave little room for interpretation, certain options like ?somewhat agree? can mean different things to different individuals. The Impact of Facial Lipofilling on Patient-Perceived Improvement in Facial Appearance and Quality of Life. Lipofilling of the Breast Does Not Increase the Risk of Recurrence of Breast Cancer: A Matched Controlled Study. Correction with autologous fat grafting for contour changes of the breasts after im plant removal in Asian women. Centrifugation versus PureGraft for fatgrafting to the breast after breast-conserving therapy. Autologous fat transplantation in patients with breast cancer: "silencing" or "fueling" cancer recurrence? Autologous fat transfer national consensus survey: trends in techniques for harvest, preparation, and application, and perception of short and long-term results. Adipose-derived stromal vascular fraction cells and platelet-rich plasma: basic and clinical evaluation for cell-based therapies in patients with scars on the face. The observation of human body adipose tissue damage degree by the method of drawing. Autologous human fat grafting: effect of harvesting and preparation techniques on adipocyte graft survival. The role of cannula diameter in improved adipocyte viability: a quantita tive analysis. Contribution of endothelial precursors of adipose tissue to breast cancer: progres sion-link with fat graft for reconstructive surgery. The Oncologic Safety of Breast Fat Grafting and Contradictions Between Basic Science and Clinical Studies: A Systematic Review of the Recent Literature. A systematic review of reliability and objective criterion-related validity of physical activity questionnaires. Despite this upsurge in scientific/clinical interest, objectifying satisfaction has only recently progressed beyond simple likert /visual analog-scales. Furthermore, differences in satisfaction between patients and surgeons has not been thoroughly studied. Method: A photo-comparison-study between European plastic surgeons and different patient-groups (1. Interrater-agreements amongst different patient-groups/ and surgeons from different countries amongst themselves was substantial to al most perfect. Finally, we found that patients are generally more optimistic about postoperative results than surgeons. However, overall patients tend to be more opti mistic about postoperative results and patient-education in general does not seem influenced by surgeon nationality. Concerning the female breast, the first description dates 1 from 1893 with Neuber attempting transfer of bulk volumes of fat. Furthermore, with the 6 first standardized protocol described by Coleman in 1995 leading to an in crease in the number of objective and reproducible study-designs the Fat Graft Task Force of the American society of Plastic surgeons, in 2009, stated that the 7 procedure was no longer prohibited. This resulted in large volume studies, systematic reviews and meta-analysis, showing the efficacy and safety in terms of improving volume retention and acceptable oncological and radiological 8-12 safety respectively. With this gradual reassurance of the safety of the tech nique, the authors believe the aim for further research is to lean more towards efficacy since this is an area where profit is still to be gained. Moreover, patient satisfac tion is being described occasionally, and only recently with the use of validated 13-16 questionnaires like the Breast-Q. Also, the satisfaction of patients and sur geons is generally reported in rates, and comparisons in the cosmetic apprecia tion of the procedure between groups of surgeons and patients based on back ground and experience has not been thoroughly studied. Plastic surgeons from ten European countries (Netherlands, Belgium, Germany, Great Britain, France, Spain, Austria, Switzerland, Italy and Greece) were contact ed either directly through their national professional organization or indirectly by email with an invitation to score the pre and postoperative photographs. In addition to the physician rating, patients from two local hospitals (VieCuri Medical Center, Venlo/ Zuyderland Medical Center, Sittard, Limburg, the Netherlands) were contacted according to the ethical guidelines from the Maastricht University Medical Center and asked for participation in this study. Emotionally unstable patients due to current or previous breast-cancer related mental trauma (as judged by the investigator) in who the photographs might aggravate anxiousness or negative emotions were excluded. Patient recruitment Group 1 and 2 patients were recruited in a retrospective matter. A recruitment letter was send by the treating physician, in which they were informed of the study and subsequently asked if they may be contacted by phone for further information and possibly inclusion (checkbox yes or no option. On accordance the patient received the questionnaire includ ing the photographs through an online (Survey Gizmo?) link followed by an informed consent letter with retour envelop send through conventional mail. Group 3 patients were included in a prospective consecutive manner in which the initial (none breast related) consultation was concluded with the treating physician inquiring if the patient was willing to participate in a study. The sampling variance of kappa was determined with the Jackknife method, as 17,18 suggested by Van belle and Albert (2009. Next to the agreement between differ ent groups of raters, the agreement between surgeons from different countries was assessed in a similar way. In addition to analyzing the interrater agreement between groups on the pre and postoperative photographs themselves, the authors wanted to examine the agreement on the increase (or possibly decrease) in cosmetic evaluation between the pre and postoperative photographs, i. Kappa was calculated for the agreement on the scoring trend between the surgeons and the patient groups and the patient groups among each other, for all sets of photographs. The difference in scoring trend per set of pre-/ postoperative photographs be tween the groups of raters was evaluated by ordinal regression analysis. Results A total of 312 plastic surgeons completed the questionnaires out of 520 and these were included for analysis. Despite the fact that surveys were distributed amongst (members of) European plastic surgery associations only, some of the respondents worked outside of Europe. Table 1 illustrates the distribution amongst countries, with most respondents practicing from the Netherlands (37. Eighty two percent completed their medical specialty, with a quarter of the respond ents having more than 20 years of practicing experience. Table 1: Participating countries and patients Surgeons Country Active vs Passive (Estimated*) emails send Number of respondents participation per country (response (overall %) rate) Netherlands Active *425 (33.
Purchase 160 mg super avana visa. Nature Crazy’s Top 6 Tips for reversing Erectile Dysfunction.
Overall requirements for commercial drivers impotence merriam webster buy 160 mg super avana fast delivery, as well as the specific requirements in the job description of the driver impotence due to diabetes cheap super avana 160mg fast delivery, should be deciding factors in the certification process erectile dysfunction proton pump inhibitors purchase super avana 160 mg with amex. Advisory Criteria/Guidance Anticoagulant Therapy the most current guidelines for the use of warfarin (Coumadin) for cardiovascular diseases are found in the Cardiovascular Advisory Panel Guidelines for the Medical Examination of Commercial Motor Vehicle Drivers erectile dysfunction treatment emedicine super avana 160mg with amex. Anticoagulant therapy may be utilized in the treatment of cardiovascular or neurological conditions xylometazoline erectile dysfunction order super avana 160 mg. The guidelines emphasize that the certification decision should be based on the underlying medical disease or disorder requiring medication erectile dysfunction protocol ingredients discount super avana 160 mg fast delivery, not the medication itself. Page 76 of 260 Aneurysms, Peripheral Vascular Disease, and Venous Disease and Treatments the diagnosis of arterial disease should alert you to the need for an evaluation to determine the presence of other cardiovascular diseases. Rupture is the most serious complication of an abdominal aortic aneurysm and is related to the size of the aneurysm. Deep venous thrombosis can be the source of acute pulmonary emboli or lead to long-term venous complications. Intermittent claudication is the primary symptom of peripheral vascular disease of the lower extremities. Detection during a physical examination depends on aneurysm size and is affected by obesity. Monitoring of an aneurysm is advised because the growth rate can vary and rapid expansion can occur. Adequate treatment with anticoagulants decreases the risk of recurrent thrombosis by approximately 80%. Waiting period No recommended time frame You should not certify the driver until etiology is confirmed, and treatment has been shown to be adequate/effective, safe, and stable. Page 78 of 260 To review the Venous Disease Recommendation Tables, see Appendix D of this handbook. Chronic Thrombotic Venous Disease Chronic thrombotic venous disease of the legs increases the risk of pulmonary emboli; however, there is insufficient research to confirm the level of risk. As a medical examiner, you must evaluate on a case-by case basis to determine if the driver meets cardiovascular requirements. Decision Maximum certification period 2 years Recommend to certify if: the driver has no symptoms. Intermittent Claudication Approximately 7% to 9% of persons with peripheral vascular disease develop intermittent claudication, the primary symptom of obstructive vascular disease of the lower extremity. In cases of severe arterial insufficiency, necrosis, neuropathy, and atrophy may occur. Waiting period Minimum 3 months for post-surgical repair You should not certify the driver until etiology is confirmed and treatment has been shown to be adequate/effective, safe, and stable. Decision Maximum certification 1 year Page 79 of 260 Recommend to certify if: the driver, following surgery has:. To review the Peripheral Vascular Disease Recommendation Table, see Appendix D of this handbook. Other Aneurysms Aneurysms can develop in visceral and peripheral arteries and venous vessels. Much of the information on aortic aneurysms is applicable to aneurysms in other arteries. Page 80 of 260 Monitoring/testing You may, on a case-by-case basis, obtain additional tests and consultations to adequately assess driver medical fitness for duty. Peripheral Vascular Disease Aneurysms can develop in visceral and peripheral arteries and venous vessels. Rupture of any of these aneurysms can lead to gradual or sudden incapacitation and death. Surgical repair of the aneurysm and meets post-surgical repair of aneurysm guidelines. Recommendation for surgical repair of an aneurysm, from a cardiovascular specialist who understands the functions and demands of commercial driving, but has not had surgical repair. Monitoring/Testing You may, on a case-by-case basis, obtain additional tests and consultations to adequately assess driver medical fitness for duty. Page 81 of 260 Post-Surgical Repair of Aneurysm With improved surgical outcomes, and without contraindication for surgery, aneurysms can be electively repaired to prevent rupture. The decision by the treating provider not to surgically repair an aneurysm does not mean that the driver can be certified to drive safely. However, a recommendation to surgically repair an aneurysm disqualifies the driver until the aneurysm has been repaired and a satisfactory recovery period has passed. Recommendation for surgical repair of an aneurysm from a cardiovascular specialist who understands the functions and demands of commercial driving, but has not had surgical repair. Monitoring/Testing When post-surgical treatment includes anticoagulant therapy, the driver should meet monitoring guidelines. Decision Maximum certification period 1 year Recommend to certify if: the driver has:. To review the Venous Disease Recommendation Tables, see Appendix D of this handbook. Waiting period No recommended time frame You should not certify the driver until etiology is confirmed and treatment has been shown to be adequate/effective, safe, and stable. Decision Maximum certification period? 2 years Recommend to certify if: the driver is otherwise medically qualified. Page 83 of 260 Monitoring/Testing You may on a case-by-case basis obtain additional tests and/or consultation to adequately assess driver medical fitness for duty. Thoracic Aneurysm While relatively rare, thoracic aneurysms are increasing in frequency. Size of the aorta is considered the major factor in determining risk for dissection or rupture of a thoracic aneurysm. Page 84 of 260 Varicose Veins Varicose veins with the associated symptoms and complications affect more than 20 million people in the United States. Complications include chronic venous insufficiency, leg ulcerations, and recurrent deep vein thrombosis. The presence of varicose veins does not medically disqualify the commercial driver. Decision Maximum certification period 2 years Recommend to certify if: the driver has no complications. Cardiac Arrhythmias and Treatment the majority of sudden cardiac deaths are thought to be secondary to ventricular tachycardia or ventricular fibrillation and occur most often when there is no prior diagnosis of heart disease. Risk determination is difficult because of the number of variables that must be considered. While defibrillation may restore a normal rhythm, there remains a high risk of recurrence. When the driver has a history of arrhythmia or uses an anti-arrhythmia device, you, as a medical examiner, should consider the following:. The management of the underlying disease is not effective enough for the driver to meet cardiovascular qualification requirements. To review the Implantable Defibrillator Recommendation Table, see Appendix D of this handbook. When assessing the risk for sudden, unexpected incapacitation in a driver with a pacemaker, the underlying disease responsible for the pacemaker indication must be considered. Currently, pacemakers and the lead systems are reliable and durable over the long term. Waiting period Minimum 1 month post-pacemaker implantation if underlying disease is:. Page 86 of 260 Minimum 3 months post-pacemaker implantation if underlying disease is:. Treatment by catheter ablation is usually curative and allows drug therapy to be withdrawn. Anticoagulant therapy decreases the risk of peripheral embolization in individuals with risk factors for stroke. See the Supraventricular Tachycardias Recommendation Table for diagnosis-specific recommendations. Waiting period Minimum 1 month anticoagulated adequately and diagnosis is atrial fibrillation. Minimum 1 month post-isthmus ablation and diagnosis is atrial flutter Minimum 1 month asymptomatic/treated asymptomatic and diagnosis is:. A driver could have a benign underlying medical problem with an excellent prognosis but still not be medically qualified as a commercial driver. For example, if a benign supraventricular arrhythmia causes syncope, the driver cannot be medically certified until the problem has been corrected. Ventricular Arrhythmias Ventricular arrhythmias are categorized as ventricular fibrillation and ventricular tachycardia and are responsible for the majority of instances of cardiac sudden death. Most cases are caused by coronary heart disease, but can also occur in people with hearts that are structurally normal. See the Ventricular Arrhythmias Recommendation Table in Appendix D of this handbook for diagnosis specific recommendations. Monitoring/Testing Have annual evaluation by a cardiovascular specialist who understands the functions and demands of commercial driving. See the Ventricular Arrhythmias Recommendation Table for diagnosis-specific recommendations. Cardiovascular Tests Detection of an undiagnosed heart or vascular finding during a physical examination may indicate the need for further testing and examination to adequately assess medical fitness for duty. Diagnostic-specific testing may be required to detect the presence and/or severity of cardiovascular diseases. The additional testing may be ordered by the medical examiner, primary care physician, cardiologist, or cardiovascular surgeon. When requesting additional evaluation from a specialist, the specialist must understand the role and function of a driver; therefore, it is helpful if you include a description of the role of the driver and a copy of the applicable medical standard(s) and guidelines with the request. Exercise Tolerance Test the exercise tolerance test is the most common test used to evaluate workload capacity and detect cardiac abnormalities. These activities include sitting, slow walking, and lifting light objects of no more than 10 pounds. Overall requirements for commercial drivers along with the specific requirements in the job description should be deciding factors in the certification process. Coronary Heart Diseases and Treatments As a medical examiner, it is your decision whether the nature and severity of the condition of the driver will result in gradual or sudden incapacitation. Page 91 of 260 Sudden death occurs when an individual goes from a usual state of health to death within 1 hour. The incidence of crashes caused by sudden death is relatively low, primarily because of the length of time between the onset of the cardiovascular event and the incapacitation of the driver. Emphasize that the driver may have only a short time following the onset of symptoms to safely stop the vehicle and call for medical assistance. Decision Maximum certification period 1 year Recommend to certify if: the driver: Page 92 of 260. The presence of this condition usually implies that at least one coronary artery has hemodynamically significant narrowing. When evaluating the driver with angina, you should distinguish between stable and unstable angina. The presence of unstable angina may be a precursor to a cardiovascular episode known to be accompanied by syncope, dyspnea, collapse, or congestive cardiac failure. Recommend not to certify if: the driver has had unstable angina within 3 months of examination. Evaluation from a cardiovascular specialist who understands the functions and demands of commercial driving. Decision Maximum certification 1 year Recommend to certify if: As the medical examiner, you believe that the nature and severity of the medical condition of the driver does not endanger the health and safety of the driver and the public. In the setting of an uncomplicated, elective procedure to treat stable angina, the post-procedure waiting period is 1 week. The waiting period allows for a small threat caused by acute complications at the vascular access site. Clearance from a cardiovascular specialist who understands the functions and demands of commercial driving. Typical angina symptoms should prompt evaluation with a stress imaging study or repeat angiography. Congenital Heart Disease Heart failure and sudden death are the major causes of death among individuals with congenital heart disease. Due to the complexity of these problems, the Cardiovascular Advisory Panel Guidelines for the Medical Examination of Commercial Motor Drivers recommend that the driver has regular, ongoing follow up by a cardiologist knowledgeable in adult congenital heart disease. Advances in surgical and medical management are expected to result in an increased number of individuals with congenital heart disease seeking driver certification. Ebstein anomaly is included in the handbook because it is a condition you are likely to encounter in the clinical setting. Ebstein Anomaly Ebstein anomaly is a congenital downward displacement of the tricuspid valve. Adults with a mild form of Ebstein anomaly can remain asymptomatic throughout their lives. Monitoring/Testing Annual cardiovascular re-evaluation should include echocardiography and evaluation by a cardiologist knowledgeable in adult congenital heart disease and who understands the functions and demands of commercial driving. To review the Congenital Heart Disease Recommendation Table, see Appendix D of this handbook. Page 100 of 260 Heart Transplantation Although the number of heart transplant recipients is relatively small, some recipients may wish to be commercial motor vehicle drivers. The major medical concerns for certification of a commercial driver heart recipient are transplant rejection and post-transplant atherosclerosis. Decision Maximum certification period 6 months Recommend to certify if: the driver:. Recommend not to certify if: As the medical examiner, you believe that the nature and severity of the medical condition endangers the health and safety of the driver and the public. Monitoring/Testing Monitoring the driver with a heart transplant should include re-evaluation and recertification every 6 months by a cardiovascular specialist who:.
Medical Management: Acute Phase During the acute phase erectile dysfunction pump order generic super avana on line, management is symptomatic and directed toward preventing or treating complications impotence law chennai purchase cheap super avana online. Pancreatitis impotence reasons and treatment generic super avana 160mg with visa, Acute 483 • Oral intake is withheld to inhibit pancreatic stimulation and secretion of pancreatic enzymes erectile dysfunction natural foods purchase super avana us. Medical Management: Postacute Phase P • Antacids are given when the acute episode begins to resolve erectile dysfunction drugs cost comparison purchase super avana without prescription. Nursing Management Relieving Pain and Discomfort • Administer analgesics as prescribed erectile dysfunction joliet discount super avana 160 mg on line. Current recommenda tion for pain management is parenteral opioids, including morphine, hydromorphone, or fentanyl via patient controlled analgesia or bolus. Improving Breathing Pattern • Maintain patient in semi-Fowlers position to decrease pres sure on diaphragm. Improving Nutritional Status • Assess nutritional status and note factors that alter the P patients nutritional requirements (eg, temperature eleva tion, surgery, drainage. Maintaining Skin Integrity • Assess the wound, drainage sites, and skin carefully for signs of infection, inflammation, and breakdown. Pancreatitis, Acute 485 Monitoring and Managing Complications Fluid and Electrolyte Disturbances • Assess fluid and electrolyte status by noting skin turgor and moistness of mucous membranes. Pancreatic Necrosis • Transfer patient to intensive care unit for close monitoring. Shock and Multiple Organ Failure • Monitor patient closely for early signs of neurologic, car diovascular, renal, and respiratory dysfunction. Promoting Home and Community-Based Care Teaching Patients Self-Care • Provide patient and family with facts and explanations of the acute phase of illness; provide necessary repetition and rein forcement. Pancreatitis, Chronic Chronic pancreatitis is an inflammatory disorder character ized by progressive anatomic and functional destruction of the pancreas. The end result is obstruc tion of the pancreatic and common bile ducts and duode num. In addition, there is atrophy of the epithelium of the ducts, inflammation, and destruction of the secreting cells of the pancreas. Alcohol consumption in Western societies and malnutrition worldwide are the major causes. The incidence of pancreatitis among alcoholics is 50 times the rate in the nondrinking population. Pathophysiology Long-term alcohol consumption causes hypersecretion of pro P tein in pancreatic secretions, resulting in protein plugs and calculi within the pancreatic ducts. Damage is more severe in patients with diets low in protein and very high or very low in fat. Because heavy drinkers usually smoke, it is difficult to separate the effects of the alcohol abuse and smoking. Clinical Manifestations • Recurring attacks of severe upper abdominal and back pain, accompanied by vomiting; opioids may not provide relief. Medical Management Treatment is directed toward preventing and managing acute attacks, relieving pain and discomfort, and managing exocrine and endocrine insufficiency of pancreatitis. P • Pain and discomfort are relieved with analgesics; yoga may be an effective nonpharmacologic method for pain reduc tion and for relief of other coexisting symptoms. Patient and family are taught the hazard of severe hypoglycemia related to alcohol use. Nursing Management See Nursing Management under Pancreatitis, Acute, for treatment guidelines. Parkinsons Disease Parkinsons disease is a slowly progressive degenerative neuro logic disorder affecting the brain centers that are responsible for control and regulation of movement. The degenerative or idiopathic form of Parkinsons disease is the most common; there is also a secondary form with a known or suspected cause. The cause of the disease is mostly unknown but research suggests several causative factors (eg, genetics, ather osclerosis, viral infections, head trauma. The disease usually first appears in the fifth decade of life and is the fourth most common neurodegenerative disease. P Pathophysiology Parkinsons disease is associated with decreased levels of dopamine resulting from destruction of pigmented neuronal cells in the substantia nigra in the basal ganglia region of the brain. The loss of dopamine stores in this area of the brain results in more excitatory neurotransmitters than inhibitory neurotransmitters, leading to an imbalance that affects vol untary movement. Cellular degeneration causes impairment of the extrapyramidal tracts that control semiautomatic func tions and coordinated movements; motor cells of the motor cortex and the pyramidal tracts are not affected. Clinical Manifestations the cardinal signs of Parkinsons disease are tremor, rigidity, bradykinesia (abnormally slow movements), and postural instability. Parkinsons Disease 489 • Resting tremors: a slow, unilateral turning of the forearm and hand and a pill-rolling motion of the thumb against the fingers; tremor at rest and increasing with concentration and anxiety. Other Characteristics • Autonomic symptoms that include excessive and uncon trolled sweating, paroxysmal flushing, orthostatic hypoten sion, gastric and urinary retention, constipation, and sexual dysfunction. Assessment and Diagnostic Methods • Patients history and presence of two of the four cardinal manifestations: tremor, rigidity, bradykinesia, and postural changes. Medical Management Goal of treatment is to control symptoms and maintain func tional independence; no approach prevents disease progression. Pharmacologic Therapy • Levodopa (Larodopa) is the most effective agent and the mainstay of treatment. Surgical Management P • Surgery to destroy a part of the thalamus (stereotactic thal amotomy and pallidotomy) to interrupt nerve pathways and alleviate tremor or rigidity. Observe the patient for quality of speech, loss of facial expression, swallowing deficits (drooling, poor head control, coughing), tremors, slowness of movement, weakness, forward posture, rigidity, evidence of mental slowness, and confusion. The following questions may facilitate observations: • Do you have leg or arm stiffness? Nursing Diagnoses • Impaired physical mobility related to muscle rigidity and motor weakness • Self-care deficits (eating, drinking, dressing, hygiene, and toileting) related to tremor and motor disturbance • Constipation related to medication and reduced activity • Imbalanced nutrition: less than body requirements related P to tremor, slowness in eating, difficulty in chewing and swallowing • Impaired verbal communication related to decreased speech volume, slowness of speech, inability to move facial muscles • Ineffective coping related to depression and dysfunction due to disease progression Other nursing diagnoses may include sleep pattern distur bances, deficient knowledge, risk for injury, risk for activity intolerance, disturbed thought processes, and compromised family coping. Nursing Interventions Improving Mobility • Help patient plan progressive program of daily exercise to increase muscle strength, improve coordination and dex terity, reduce muscular rigidity, and prevent contractures. Teach patient to walk erect, watch the horizon, use a wide-based gait, swing arms with walking, walk heel-toe, and practice marching to music. Also encourage breathing exercises while walking and frequent rest periods to prevent fatigue or frustration. P Enhancing Self-Care Activities • Encourage, teach, and support patient during activities of daily living. Improving Swallowing and Nutrition • Promote swallowing and prevent aspiration by having patient sit in upright position during meals. Parkinsons Disease 493 • Teach patient to place the food on the tongue, close the lips and teeth, lift the tongue up and then back, and swallow; encourage patient to chew first on one side of the mouth and then on the other. Encouraging Use of Assistive Devices • An occupational therapist can assist in identifying appro priate adaptive devices. Improving Communication • Remind patient to face the listener, speak slowly and deliberately, and exaggerate pronunciation of words; a small electronic amplifier is helpful if the patient has diffi culty being heard. Supporting Coping Abilities • Encourage faithful adherence to exercise and walking program; point out activities that are being maintained through active participation. The education plan should include a clear explanation of the disease and the goal of assisting the patient to remain functionally independent as long as possible. Make every effort to explain the nature of 494 Pelvic Infection (Pelvic Inflammatory Disease) the disease and its management, to offset disabling anxieties and fears. The patient and family also need to know about the effects and side effects of medications and the importance of reporting side effects to the physician. Evaluation Expected Patient Outcomes • Strives toward improved mobility • Progresses toward self-care • Maintains bowel function P. Attains improved nutritional status • Achieves a method of communication • Copes with effects of Parkinsons disease For more information, see Chapter 65 in Smeltzer, S. Infection, which may be acute, subacute, recurrent, or chronic and localized or widespread, is usually caused by bacte ria but may be attributed to a virus, fungus, or parasite. Pathophysiology Pathogenic organisms usually enter the body through the vagina, pass through the cervical canal into the uterus, and may proceed to one or both fallopian tubes and ovaries, and into the pelvis. Complications • Pelvic or generalized peritonitis, abscesses, strictures, and fallopian tube obstruction • Adhesions that eventually may require removal of the uterus, tubes, and ovaries • Bacteremia with septic shock and thrombophlebitis with possible embolization Medical Management Broad-spectrum antibiotic therapy is instituted, with mild to moderate infections being treated on an outpatient basis. If 496 Pelvic Infection (Pelvic Inflammatory Disease) the patient is acutely ill, hospitalization may be required. Nasogastric intuba tion and suction are used if ileus is present; vital signs are monitored. Nursing Management Nursing measures include nutritional support of the patient and administration of antibiotic therapy as prescribed. Vital signs are assessed, as are characteristics of the disorder and the amount of vaginal discharge. Comfort measures include applying heat safely to the abdomen and administering analgesic agents for pain relief. Another nursing intervention is prevention of transmission of infection to others by impeccable hand hygiene and use of barrier precautions and hospital guidelines for disposing of bio hazardous articles (eg, pads. While in bed, they remain in semi-Fowlers position to facilitate dependent drainage. Before discharge, patients are taught self care measures: • Inform patient of the need for precautions and encourage her P to take part in procedures to prevent infecting others and pro tect herself from reinfection. Stress that if a partner is not well known to her or has had other sexual partners recently, use of condoms is essential to prevent infection and sequelae. Pemphigus 497 • Teach patient to consult with health care provider if unusual vaginal discharge or odor is noted. Pemphigus Pemphigus is a group of serious diseases of the skin charac terized by the appearance of bullae (blisters) on apparently normal skin and mucous membranes (mouth, vagina. Evi dence indicates that pemphigus is an autoimmune disease involving immunoglobulin G (IgG. The condi tion may be associated with ingestion of penicillin and cap topril and with myasthenia gravis. Genetic factors may also play a role, with the highest incidence in those of Jewish or Mediterranean descent. Clinical Manifestations • Most cases present with oral lesions appearing as irregularly shaped erosions that are painful, bleed easily, and heal slowly. Fluid and electrolyte imbalance and hypoalbuminemia may result from loss of fluid and protein. Assessment and Diagnostic Findings Diagnosis is confirmed by histologic examination of a biopsy specimen and immunofluorescent examination of the serum, which show circulating pemphigus antibodies. Medical Management Goals of therapy are to bring the disease under control as rap idly as possible, prevent loss of serum and development of sec ondary infection, and promote reepithelialization of the skin. Diagnosis Nursing Diagnoses • Acute pain of oral cavity and skin related to blistering and erosions • Impaired skin integrity related to ruptured bullae and denuded areas of skin Pemphigus 499 • Anxiety and ineffective coping related to appearance of skin and no hope of a cure • Deficient knowledge about medications and side effects Collaborative Problems/Potential Complications • Infection and sepsis related to loss of protective barrier of skin and mucous membranes • Fluid volume deficit and electrolyte imbalance related to loss of tissue fluids Planning and Goals the major goals may include relief of discomfort from lesions, skin healing, reduced anxiety and improved coping capacity, and absence of complications. Nursing Interventions Relieving Oral Discomfort • Provide meticulous oral hygiene for cleanliness and regen eration of epithelium. Enhancing Skin Integrity and Relieving Discomfort P • Provide cool, wet dressings or baths (protective and soothing. Reducing Anxiety • Demonstrate a warm and caring attitude; allow patient to express anxieties, discomfort, and feelings of hopelessness. Achieving Fluid and Electrolyte Balance • Administer saline infusion for sodium chloride depletion. Evaluation Expected Patient Outcomes • Achieves relief from pain of oral lesions • Achieves skin healing • Experiences decreased anxiety and increased ability to cope • Experiences no complications Peptic Ulcer 501 For more information, see Chapter 56 in Smeltzer, S. Peptic Ulcer A peptic ulcer is an excavation formed in the mucosal wall of the stomach, pylorus, duodenum, or esophagus. It is frequently referred to as a gastric, duodenal, or esophageal ulcer, depend ing on its location. Chronic ulcers usually occur in the lesser curvature of the stomach, near the pylorus. Peptic ulcer has been associated with bacterial infec tion, such as Helicobacter pylori. Esophageal ulcers result from the backward flow of P hydrochloric acid from the stomach into the esophagus. Zollinger–Ellison syndrome (gastrinoma) is suspected when a patient has several peptic ulcers or an ulcer that is resistant to standard medical therapy. This syndrome involves extreme gastric hyperacidity (hypersecretion of gastric juice), duodenal ulcer, and gastrinomas (islet cell tumors. These patients may have coex istent parathyroid adenomas or hyperplasia and exhibit signs of hypercalcemia. Stress ulcer (not to be confused with Cushings or Curlings ulcers) is a term given to acute mucosal ulceration of the duo denal or gastric area that occurs after physiologically stressful 502 Peptic Ulcer events, such as burns, shock, severe sepsis, and multiple organ trauma. Fiberoptic endoscopy within 24 hours of trauma or injury shows shallow erosions of the stomach wall; by 72 hours, multiple gastric erosions are observed, and as the stressful con dition continues, the ulcers spread. When the patient recovers, the lesions are reversed; this pattern is typical of stress ulcer ation. Clinical Manifestations • Symptoms of an ulcer may last days, weeks, or months and may subside only to reappear without cause. Assessment and Diagnostic Methods • Physical examination (epigastric tenderness, abdominal dis tention. Pharmacologic Therapy • Antibiotics combined with proton pump inhibitors and bis muth salts to suppress H. The patient needs to identify situations that are stressful or exhausting (eg, rushed lifestyle and irregular schedules) and implement changes, such as establishing regular rest periods during the day in the acute phase of the disease.