Neal H Cohen, MD, MS, MPH
- Professor, Department of Anesthesia and Perioperative Care, University of California, San Francisco, School of Medicine, San Francisco, California

https://profiles.ucsf.edu/neal.cohen
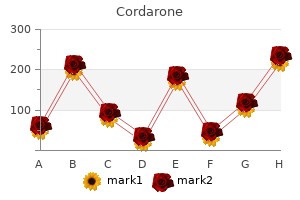
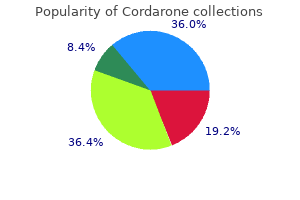
Keep the tube for 10 days medicine allergy buy cordarone 100mg on-line, and check it daily by since parasitic forms are more resistant to slight withdrawing a small amount of fluid from the bot acidity than are free-living forms symptoms 8 days after ovulation cheap cordarone on line. Examine the larvae for motility and typical the volume accordingly to achieve a 1:30 dilution morphological features to reveal whether hook of acid) medications emts can administer discount cordarone 250 mg on-line. Free-living nematodes are killed medications heart disease cordarone 100mg fast delivery, while worm medications ms treatment effective cordarone 200 mg, Strongyloides medications japan purchase cordarone with visa, or Trichostrongylus larvae parasitic species live for about 24 h. Larvae of certain Results and Patient Reports from Harada-Mori species are susceptible to cold environments. If Strongyloides (Petri Dish) organisms are present, free-living stages and larvae may be found after several days in culture. As with previ Example: Strongyloides stercoralis larvae detected ous techniques, sufficient moisture is provided by con by fecal culture tinuous soaking of the filter paper in water. Fresh stool material is placed on the filter paper, which is cut to fit Procedure Notes for Harada-Mori Filter Paper the dimensions of a standard (1 by 3-in. The filter paper is then placed on a slanted glass slide in a glass or plastic petri dish containing water. If the larvae are too active to observe under the technique allows direct examination of the culture sys microscope and morphologic details are difficult tem with a dissecting microscope to look for nematode to see, the larvae can be heat killed within the tube larvae and free-living stages of S. Since infective larvae may migrate upward as Quality Control for the Filter Paper/Slant Culture well as downward on the filter paper strip, cau Technique (Petri Dish) tion must be exercised in handling the fluid and the paper strip itself to prevent infection. Wear gloves when and handling of fresh fecal specimens for parasito handling the cultures. Fresh stool is required for this procedure; pre make sure that the procedure is precise. The microscope should be calibrated, and the objectives and oculars used for the calibration Procedure Limitations for Harada-Mori Filter procedure should be used for all measurements Paper Strip Culture on the microscope. The Harada-Mori technique allows both objectives should be posted on the microscope for parasitic and free-living forms of nematodes to easy access (multiplication factors can be pasted develop. It is important to maintain the original water level Technique (Petri Dish) to keep optimum humidity. Preserved fecal specimens or specimens obtained film of 1 to 2 g of fresh fecal material in the center after a barium meal are not suitable; fresh stool of the strip. Place the slide inclined at one end of the petri dish by resting Procedure Limitations for the Filter Paper/Slant the slide on a piece of glass rod or glass tubing; Culture Technique (Petri Dish) identify the specimen on the dish (Figure 28. The filter paper/slant culture technique allows tom one-fourth of the slide is immersed in water. As with soil or water containing these forms, it may needed, add water to maintain the original level. This distinction is possible since parasitic with the dissecting microscope or by withdraw forms are more resistant to slight acidity than are ing a small amount of fluid and placing it on a free-living forms. Larvae of certain spe Results and Patient Reports from the Filter Paper/ cies are susceptible to cold environments. If Strongyloides organ isms are present, free-living stages and larvae may be Another way to culture hookworm, Strongyloides, and found after several days in culture. The conditions of this culture provide an environment detected at the end of incubation. It provides an efficient way to harvest large numbers of Example: Strongyloides stercoralis larvae detected infective-stage larvae for use in experimental infections. Follow routine procedures for optimal collection Technique (Petri Dish) and handling of fresh fecal specimens for parasito 1. Examine known positive and negative samples of slight heating can be used to kill the larvae. Infective larvae may be found any time after the make sure that the procedure is precise. The microscope should be calibrated, and the objec must be exercised in handling the fluid and the tives and oculars used for the calibration procedure paper strip itself to prevent infection. Wear gloves should be used for all measurements on the micro when handling the cultures. There may be infective larvae in the moisture that should be posted on the microscope for easy access accumulates under the petri dish lid, so be care (multiplication factors can be pasted on the body of ful not to allow the water to touch the skin when the microscope). Additional Techniques for Stool Examination 835 Procedure for Charcoal Culture organisms are present, free-living stages and larvae may 1. Mix 20 to 40 g of fresh fecal material in tap water be found after several days in culture. Mix thoroughly Example: Strongyloides stercoralis larvae detected with a wooden tongue depressor until the fecal sus by fecal culture pension is evenly distributed throughout the moist ened charcoal. Water can be added to ensure that there is adequate moisture, but do not add so much Procedure Notes for Charcoal Culture water than it forms a layer on the bottom of the 1. Cover the dish, and place it in the dark (in a slight heating can be used to kill the larvae. Check the dish the next day to make sure that fourth day and occasionally after the first day there is still sufficient moisture. Since infective larvae may coal still glistens); if water is needed, sprinkle it on be present, use caution when handling the fluid, the surface without further mixing. It is important to maintain the moisture on the mulate on the underface of the lid, and it may charcoal to keep optimum humidity (the charcoal contain infective-stage larvae. Preserved fecal specimens or specimens obtained been prepared, hookworm and Strongyloides lar after a barium meal are not suitable; fresh stool vae will have reached the infective stage. To harvest the larvae, prepare a round gauze pad Procedure Limitations for Charcoal Culture of 10 to 12-layer thickness stapled at the edges 1. If specimens have ping wet), and apply it carefully with forceps so been contaminated with soil or water containing that it snugly covers the surface of the charcoal. Expose the dish, with lid off, to a light source such slight acidity than are free-living forms. After approximately 1 h, the pad can be carefully the volume accordingly to achieve a 1:30 dilution removed with forceps and inverted onto the sur of acid). Free-living nematodes are killed, while face of water in a pilsner glass filled with water. Specimens that have been refrigerated or preserved larvae will now make their way through the pad, are not suitable for culture. Larvae of certain spe enter the water, and fall to the bottom of the glass, cies are susceptible to cold environments. With care, there will be no charcoal at the bottom of the glass, and the larvae Baermann Technique will form a clean sediment. Another method of examining a stool specimen suspected of containing small numbers of Strongyloides larvae is the Results and Patient Reports from Charcoal Culture use of a modified Baermann apparatus (Figure 28. If Strongyloides relies on the principle that active larvae will migrate from 836 Chapter 28 a fresh fecal specimen that has been placed on a wire mesh with several layers of gauze which are in contact with tap water (2, 7, 28). Larvae migrate through the gauze into the water and settle to the bottom of the funnel, where they can be collected and examined. The main difference between this method and the Harada-Mori and petri dish methods is the greater amount of fresh stool used, possi bly providing a better chance of larval recovery in a light infection. Besides being used for patient fecal specimens, this technique can be used to examine soil specimens for the presence of larvae. Follow routine procedures for optimal collection and handling of fresh specimens for parasitologic examination. Examine known positive and negative samples of stools (from laboratory animals), if available, to make sure that the procedure is precise. The microscope should be calibrated, and the objectives and oculars used for the calibration procedure should be used for all measurements on the microscope. The calibration factors for all objectives should be posted on the microscope for easy access (multiplication factors can be pasted on the body of the microscope). If possible, use a fresh fecal specimen that has been obtained after administration of a mild saline cathartic, not a stool softener. Close the pinch clamp at the bottom of the tubing, and fill the funnel with tap water until it just soaks the gauze padding. Spread a large amount of fecal material on the the microscope (magnification, 100 and 400) gauze padding so that it is covered with water. Allow the apparatus to stand for 2 h or longer; before slowly releasing the pinch clamp. Infective then draw off 10 ml of fluid into the beaker by larvae may be present; wear gloves when perform releasing the pinch clamp, centrifuge the fluid for ing this procedure. Additional Techniques for Stool Examination 837 Results and Patient Reports from the Modification of the Baermann Method Baermann Technique A simple modification of the Baermann method for diag Larval nematodes (hookworm, S. Both infective and modification, the funnel used in the original version is noninfective Strongyloides larvae may be recovered, par replaced by a test tube with a rubber stopper, perforated ticularly in a heavy infection. Although the method is almost identical to the original Baermann method, the amount of Procedure Notes for the Baermann Technique stool used in the modified method is smaller. It may be difficult to observe morphologic details in rapidly moving larvae; a drop of iodine or formalin Agar Plate Culture for or slight heating can be used to kill the larvae. Infective larvae may be found any time after the fourth day and occasionally after the first day in Agar plate cultures are also recommended for the recovery heavy infections. Preserved fecal specimens or specimens obtained after a barium meal are not suitable for process Figure 28. The Baermann technique allows both parasitic and free-living forms of nematodes to develop. If specimens have been contaminated with soil or water containing these forms, it may be necessary to distinguish parasitic from free-living forms. This distinction is possible since parasitic forms are more resistant to slight acidity than are free-living forms. Release the pinch clamp slowly to prevent splash ing; have the end of the tubing close to the bottom of the beaker for the same reason. Daily search for furrows on agar plates for up to six con secutive days results in increased sensitivity for diagnosis of both S. Stool is placed onto agar plates, and the plates are sealed to prevent accidental infections and held for 2 days at room temperature. As the larvae crawl over the agar, they carry bacteria with them, thus creating visible tracks over the agar (Figure 28. The plates are examined under the microscope for confirmation of the presence of larvae, the surface of the agar is then washed with 10% formalin, and final confirmation of larval identification is made via wet examination of the sediment from the formalin washings (Figure 28. Occasionally, finding nematode larvae in sputum or bronchoalveolar lavage fluid specimens may be very suggestive of a potential infection with S. Once larvae are seen in respiratory being distributed over the plate by the movement of the larval worms. The microscope should be calibrated, and the objectives and oculars used for the calibration Note Positive tracking on agar plates has been seen on a procedure should be used for all measurements number of different types of agar. Follow routine procedures for optimal collection and handling of fresh fecal specimens for parasito logic examination. Examine agar plates to ensure that there is no Strongyloides stercoralis cracking and the agar pour is sufficient to prevent 1. Also, make sure that there is no excess ter of the agar plate (area approximately 1 in. After 2 days, examine the sealed plates through the tracks on agar plates for up to six consecutive days plastic lid under the microscope for microscopic results in increased sensitivity for diagnosis of both colonies that develop as random tracks on the agar S. When 840 Chapter 28 Results and Patient Reports from Agar Plate Culture for Strongyloides stercoralis Larval nematodes of hookworm, S. If Strongyloides organ isms are present, free-living stages and larvae may be found after several days on the agar plates. If the larvae are too difficult to observe under the microscope and morphologic details are difficult to see, the larvae can be formalin killed within the plate and examined in the formalin-concentrated sediment. Infective larvae may be found any time after the first or second day or even on the first day in a heavy infection. Do not incubate or refrigerate them at any time; this also applies to the fresh stool trying to rule out strongyloidiasis in immunocom specimen. Fresh stool is required for this procedure; pre immunosuppressive drugs, it is recommended that served fecal specimens or specimens obtained after two plates be set up, one that can be examined a barium meal are not suitable. With the ends of hot forceps, make a hole in the Procedure Limitations for Agar Plate Culture for top of the plastic petri dish. The agar plate culture technique is successful if onto the agar surface, and swirl to cover the surface any larvae present are viable. Prepare a wet smear preparation from the sedi Estimation of Worm Burdens ment and examine with a 10 objective (low power) for presence of larvae. If larvae are found, the only human parasites for which it is reasonably confirm the identification with a 40 objective possible to correlate egg production with adult worm (high dry power). Specimen Any stool specimen that is fresh and has not been refrigerated can be used. Examination Daily checking of the fluid for the presence of larvae; hold the cultures for 10 days before submitting the final report. When trying to rule out strongyloidiasis in immunocompromised patients or in those who may receive immunosuppressive drugs, it is recommended that two plates be set up, one that can be examined after 2 days and one that can be examined after the full 6 days. Results and the failure to recover larvae does not completely rule out the possibility of infection; Laboratory Reports however, the probability of infection is very low when results are negative.
However treatment variable order cordarone 100mg with mastercard, it should be ascertained that the responses are the result of chemical exposure schedule 8 medications list buy cheap cordarone 250 mg on-line. Generally medications you cant drink alcohol with cheap cordarone generic, such substances are expected to produce significant effects on the skin medicine bobblehead fallout 4 safe 100mg cordarone. In the absence of any other information medications just for anxiety buy cheap cordarone on-line, a substance is considered corrosive (Skin Category 1) if it the irritation category is that at least 2 of 3 tested animals have a mean score of 2 medications 2 times a day purchase cordarone with a visa. However, if consideration of acid/alkaline reserve suggests the substance may not be category, the mean score cut-off values are 1. If a substance is highly toxic by the dermal route, a skin corrosion/irritation study may not be practicable since the amount of test substance to be applied would 3. When observations are criterion accommodates cases when there is a significant irritant response but less than the mean score criterion for a made of skin corrosion/irritation in acute toxicity studies and are observed up through the limit dose, these data may be positive test. Solid substances (powders) elevated mean score throughout the study, including lesions persisting at the end of an observation period of normally may become corrosive or irritant when moistened or in contact with moist skin or mucous membranes. Addition of this criterion increases the sensitivity of the classification system. Test materials in the corrosive despite the low or high pH value, this needs to be confirmed by other data, preferably by data from an irritation category are excluded from the mild irritation category. Although information might be gained from the evaluation of single parameters within a tier (see 3. This is especially true when there is conflict in information available on some parameters. In the absence of any other information, a response mixture is considered corrosive (Skin Category 1) if it has a pH 2 or a pH 11. However, if consideration of acid/alkaline reserve suggests the mixture may not be corrosive despite the low or high pH value, this needs to be 4: pH-based assessment (with pH 2 or 11. This ensures that the classification process uses the available data to the greatest extent possible in characterizing the hazards 5: Validated Structure Activity Skin corrosive Deemed to be skin of the mixture without the necessity for additional testing in animals. All rights reserved (c) All existing animal data should be carefully reviewed to determine if sufficient skin corrosion/irritation evidence Figure 3. In evaluating such data, however, the reviewer should bear in mind that the reporting of dermal lesions may be incomplete, testing and observations may be made on a species other than the rabbit, and species Step Parameter Finding Conclusion may differ in sensitivity in their responses; 1a: Existing human or animal skin Skin corrosive Classify as skin a b (d) Evidence from studies using validated protocols with isolated human/animal tissues or other, non-tissue-based, corrosion/irritation data corrosive though validated, protocols should be assessed. Presently there is no validated and internationally accepted method for assessing this parameter; 1c: Existing human or animal skin Not a skin corrosive or skin Not classified a (f) All information that is available should be considered and an overall determination made on the total weight of corrosion/irritation data irritant evidence. Negative results from applicable validated No/Insufficient data skin corrosion/irritation in vitro tests are considered in the total weight of evidence evaluation. If the latter occurs, a new classification is animal studies conducted according to validated and internationally accepted test methods. In those cases the tiered weight of evidence approach should be applied as described in 3. Category 1 Category 2 Category 3 they are in the same hazard category and are not expected to affect the skin corrosion/irritation (see note below) potential of B. Where the sum of 1A ingredients is 5% but the sum of 1A+1B ingredients is of the mixture 5%, the mixture should be classified as sub-category 1B. A weighting factor of 10 is used for corrosive ingredients when they are present at a concentration below the concentration limit for classification with Category 1, but are at a concentration that will Base with pH 11. The mixture is classified as corrosive or irritant to skin Other corrosive (Category 1) ingredient 1% Category 1 when the sum of the concentrations of such ingredients exceeds a cut-off value/concentration limit. For mixtures containing strong acids or bases the pH should be used as classification criteria (see 3. A mixture containing corrosive or irritant ingredients that cannot be classified based on the additivity approach shown in Table 3. All rights reserved tested mixture classified for skin irritation (Category 2) is concentrated and does not contain skin corrosive ingredients, approach unworkable, should be classified as skin corrosion Category 1 if it contains 1% of a corrosive ingredient and the more concentrated untested mixture should be classified for skin irritation (Category 2) without additional testing. On occasion, when it is expected that concentrations in mixtures A and B, then mixture C is assumed to be in the same skin corrosion/irritation category as A the skin corrosion/irritation of an ingredient will not be evident when present at a level above the generic concentration and B. Skin Category 1 5% 1% but < 5% If mixture (i) or (ii) is already classified based on test data, then the other mixture can be classified in Skin Category 2 10% 1% but < 10% the same hazard category. Where at least hazards of mixtures, the following assumption has been made and is applied where appropriate in the tiered approach: one relevant ingredient in a mixture is classified as Category 1 without sub-categorisation, the mixture should be classified as Category 1 without sub-categorisation if the sum of all ingredients corrosive to skin is 5%. Other irritant (Category 2/3) ingredient, including acids and bases 3% Category 2/3 3. No not possible contains examples of precautionary statements and pictograms which can be used where allowed by the competent authority. Annex 3 Substance: Are there data/information to evaluate skin corrosion/irritation The table below presents specific label elements for substances and mixtures that are classified as irritating or corrosive to the skin based on the criteria set forth in this chapter. Mixture: Does the mixture as a whole or its ingredients have Classification data/information to evaluate skin corrosion/irritation It is strongly recommended that the person responsible for classification study the criteria (c) other existing animal data indicating skin corrosion after single or repeated before and during use of the decision logics. No Category 3 No symbol Is the substance or mixture a mild irritant considering criteria in Yes 3. Warning No Not classified 1 Taking into account consideration of the total weight of evidence as needed. Guidance on how to classify based on existing data from studies with 4 or more animals is given in the following paragraphs. Category 2 3,4 Does the mixture contain 3% of an ingredient which is irritant 3. Yes category 3 Does the mixture contain one or more corrosive or irritant ingredients when the additivity approach applies (see 3. Danger No No Not classified 5 3 Category 1 Does the mixture contain one or more corrosive ingredients when 3 4 Footnotes the additivity approach applies (see 3. It has been identified that some older test methods may have used up to 6 animals. Eye irritation refers to the production of changes in the eye, which are fully reversible, occurring after 3. In a total weight of evidence approach all available information bearing on the determination of (b) the substance or mixture is classified as skin irritation Category 2 if at least 3 out of 4 animals serious eye damage/eye irritation is considered together, including the results of appropriate validated in vitro tests, show a mean score per animal of 2. These observations include animals with grade 4 cornea lesions and other severe reactions. In this context, persistent lesions are considered those which are not fully reversible within an observation period of normally 21 days. Classification results directly when the animal after exposure up to 4 hours in duration; data satisfy the criteria. In other cases, classification of a substance or a mixture is made on the basis of the weight of evidence within a tier. Hazard classification as Category 1 also contains substances fulfilling the criteria of corneal opacity 3 or iritis > 1. In the absence of any other information, a substance is considered to cause the use of human data is addressed in 3. When a chemical is classified as Category 2, without further categorization, of-evidence decision about hazard assessment and hazard classification (ideally without conducting new animal tests). For substances inducing eye irritant effects reversing within an observation time of 7 days, Category 2B applies. Category 1: Serious eye (a) in at least one animal effects on the cornea, iris or conjunctiva that are not expected to 3. Possible skin corrosion has to be evaluated prior to consideration of any testing for effects on the eye and/or serious eye damage/eye irritation in order to avoid testing for local effects on eyes with skin corrosive substances. Generally such substances are expected to a produce significant effects on the eyes. This is especially true when there is and 2B are provided: conflict in information available on some parameters. Category 2B Within Category 2A an eye irritant is considered mildly irritating to eyes (Category 2B) when the effects listed above are fully reversible within 7 days of observation. All rights reserved (a) Existing human or animal data could be derived from single or repeated exposure(s), for example in Figure 3. Although human data from accident or poison centre databases can provide evidence for classification, absence of incidents is Step Parameter Finding Conclusion not itself evidence for no classification as exposures are generally unknown or uncertain; 1a: Existing human or animal Serious eye damage Classify as causing serious eye (b) Classify in the appropriate category as applicable; serious eye damage/eye damage a irritation data b (c) Existing animal data should be carefully reviewed to determine if sufficient serious eye damage/eye irritation Eye irritant Classify as eye irritant evidence is available through other, similar information. It is recognized that not all skin irritants are eye Negative data/Insufficient irritants. Expert judgment should be exercised prior to making such a determination; data/No data (d) Evidence from studies using validated protocols with isolated human/animal tissues or other non-tissue-based, 1b: Existing human or animal data, Skin corrosion Deemed to cause serious eye validated protocols should be assessed. Examples of internationally accepted, validated test methods for skin corrosion damage identifying eye corrosives and severe irritants. Presently there are no validated and internationally accepted in vitro test methods for identifying data/No data eye irritation. A positive test result from a validated in vitro test on skin corrosion would lead to the conclusion to classify as causing serious eye damage; 1c: Existing human or animal Existing data showing Not classified serious eye damage/eye that substance does not a (e) Measurement of pH alone may be adequate, but assessment of acid/alkaline reserve (buffering capacity) would irritation data cause serious eye be preferable. Presently, there is no validated and internationally accepted method for assessing this parameter; damage or eye irritation (f) All information that is available on a substance should be considered and an overall determination made on the total weight of evidence. This is especially true when there is conflict in information available on some No/Insufficient data parameters. The weight of evidence including information on skin irritation may lead to classification for eye irritation. Negative results from applicable validated in vitro tests are considered in the total weight of evidence 2: Other, existing skin/eye data in Yes; other existing data May be deemed to cause serious c evaluation. In the absence of any other information, a mixture is considered to cause serious eye damage (Eye Category 1) if it has a pH 2 or 11. This ensures that the classification process uses the available data to the greatest extent Severe damage to eyes Deemed to cause serious eye possible in characterizing the hazards of the mixture without the necessity for additional testing in animals. However, if consideration of alkali/acid reserve suggests the mixture may not cause serious eye damage despite the low 4: pH-based assessment (with pH 2 or 11. If a tested mixture classified for eye irritation (Category 2 or 2A) is concentrated and does not contain serious eye damage 3. Classification of mixtures with ingredients for which the intermediate to the concentrations in mixtures A and B, then mixture C is assumed to be in the same serious eye approach in Table 3. On occasion, when it is expected that the skin corrosion/irritation or the irreversible/reversible eye effects of an ingredient will not be evident when present at a level above the generic (a) Two mixtures: (i) A +B concentration/cut-off levels mentioned in Tables 3. A weighting factor of 10 is used for when produced by or under the control of the same manufacturer, unless there is reason to believe there is significant corrosive and serious eye damaging ingredients when they are present at a concentration below the concentration limit variation such that the serious eye damage/eye irritation potential of the untested batch has changed. If the latter occurs, for classification with Category 1, but are at a concentration that will contribute to the classification of the mixture as a new classification is necessary. The mixture is classified as seriously damaging to the eye or eye irritant when the sum of the concentrations of such ingredients exceeds a threshold cut-off value/concentration limit. For mixtures containing strong acids or bases the pH should be used as classification criterion (see 3. A mixture containing corrosive or serious eye damaging/eye irritating ingredients that cannot be classified based For three mixtures (A, B and C) with identical ingredients, where mixtures A and B have been tested on the additivity approach applied in Table 3. In these cases the mixture could be classified according to those data (see also 1. In those (ii) C + B; cases, the tiered weight of evidence approach should be applied as referred to in section 3. No not possible Hazard statement Causes serious eye damage Causes serious eye irritation Causes eye irritation a Where a chemical is classified as skin Category 1, labelling for serious eye damage/eye irritation may be Yes Mixture: Does the mixture as a whole or its ingredients omitted as this information is already included in the hazard statement for skin Category 1 (Causes severe skin burns have data/information to evaluate serious eye damage/eye Classification No and eye damage) (see Chapter 1. It is strongly recommended that the person responsible for classification study the criteria contains examples of precautionary statements and pictograms which can be used where allowed by the competent before and during use of the decision logics. No 4,5 Category 1 No Does the mixture contain 1% of an ingredient which causes serious eye damage (see 3. No Warning No 4 Category 1 Does the mixture contain one or more ingredients corrosive or seriously damaging to the eye when the additivity approach applies (see 3. Danger No 6 Category 2/2A 4,5 Does the mixture contain 3% of an ingredient which is an eye irritant (see 3. Warning No 4 Does the mixture contain one or more ingredients corrosive or seriously 6 Category 2/2A damaging to the eye/eye irritant when the additivity approach applies (see 3. Evaluation of a 4, 5 or 6 animal (a) the substance or mixture is classified as serious eye damage Category 1 if: study should follow the criteria in the following paragraphs, depending on the number of animals tested. Scoring should be done at 24, 48 and 72 hours after instillation of the test material. Skin sensitization refers to an allergic response occurring after skin contact with a substance or a mixture. For skin sensitization, an induction phase is required in which the immune system learns to react; clinical symptoms can then arise when subsequent exposure is sufficient to elicit a visible skin reaction (elicitation phase). As a consequence, predictive tests usually follow this pattern in which there is an induction phase, the response to which is measured by a standardized elicitation phase, typically involving a patch test. The local lymph node assay is the exception, directly measuring the induction response. Evidence of skin sensitization in humans normally is assessed by a diagnostic patch test.
The nurse should review the results of previous lab work with the patient and communicate with the prescriber to ensure that routine monitoring labs are done as ordered medicine bobblehead fallout 4 generic cordarone 250mg fast delivery. It is important for the nurse to listen to the patient and ensure that established routines are followed to avoid causing undue stress medications j-tube cheap cordarone online visa. Children medicine 3604 generic 100 mg cordarone visa, in particular medications you cant take while breastfeeding cordarone 100mg for sale, may have routines in place to assist them in dealing with both the physical and psychological impacts of infusions medications to treat anxiety purchase cordarone online pills. I M M U N E D E F I C I E N C Y F O U N D A T I O N | 1 7 Key Intra-infusion Assessments I Assess the patient to ensure that the infusion is being tolerated medicine engineering order 250mg cordarone overnight delivery. Key Post-infusion Assessments I Assess for any problems occurring after the infusion which may be infusion related. I Assess the need for premedications for future infusions and ensure that the premedications will be available for the next infusion. It is important for the patient to know when the next infusion is due and what his/her responsibilities regarding this infusion are. There are multiple factors to consider when choosing the route of administration; careful consideration of these factors and their relationship to the individual patient is critical to ensuring success. There is a peak in the level of IgG when the infusion is given and then the level declines to a trough before the next infusion, so there is a predictable rise and fall in levels. I Comorbidities: Does the patient have another illness which will be affected by therapy The American Academy of Allergy, Asthma and Immunology strongly discourages the use of permanent indwelling ports or central venous lines in antibody decient patients due to the risk of infection and thrombotic events. I Availability of Nursing Resources: Home infusion nursing services are not always available in every area of the country and patients may not live close to infusion centers, making self-infusion a desirable alternative. It is well tolerated by the majority of patients, but it is important to note that, just as each patient may require a different immunoglobulin product, each may also require an individualized infusion regimen in order to achieve the desired therapeutic response. Once a successful regimen has been developed, it should be carefully followed with every infusion. This includes not only the rate of the infusion and necessary premedications, but the specic product, as well. Should medications be required prior to or during an infusion, it is recommended to ush the line with at least 5-10 ml of compatible uid prior to administering the medication. If a product change is necessary, the process for assessment of tolerability and potential rate increases must again be taken slowly. I Assess the vital signs prior to each rate change to ensure that the infusion is being tolerated. Hyper or hypotension, increased heart rate, increased respiratory rate or effort, and fever could all be signs of problems. It is important to assess the clinical relevance of any alterations in vital signs. For example, if a comfortable patient falls asleep, his/her blood pressure, heart rate and respiratory rate may decrease and may not represent a pathologic concern. Similar ndings in another patient may be signs of signicant problems with the infusion. I Assess the need for comfort measures during the infusion, particularly if side effects occur. Both pharmacologic and non pharmacologic interventions (supplying blankets or pillows, heating pads and encouraging the use of relaxation techniques) may be indicated. Although true IgE medicated anaphylaxis in antibody decient patients is rare, if a patient has difculty breathing, signs of tongue or throat swelling, a feeling that the throat is closing, stridor, wheezing and/or chest tightness, generalized urticaria, or extreme anxiety, the infusion should be stopped and immediate emergency treatment, including calling 911, should be initiated. These reactions can range from mild to severe; however, most reactions occur during the initial 30 to 60 minutes of the infusion and are mild and self-limited. These reactions include anaphylactoid problems such as headaches, chills and rigors; allergic reactions like urticaria and, potentially, anaphylaxis; and other problems such as aseptic meningitis. The most common problems are related to the rate of the infusion and the temperature of the product. Reactions are more frequent with patients who are therapy naive, when therapy is given with a different product than the patient has previously been used to receiving, and/or in those who are not truly antibody decient or those who have been off of therapy for a period of time. It is important to note that most reactions occur during the initial 30 to 60 minutes of the infusion and are mild and self-limited. Types of Adverse Reactions I Pyogenic Reactions: these reactions are marked by a signicant rise in temperature and are usually accompanied by other systemic symptoms. Management of acute pyogenic reactions includes the use of antipyretic medications such as acetaminophen or ibuprofen. Patients may describe an uncomfortable feeling, such as a tightening around the neck, chest or abdomen. Other symptoms may include wheezing, ushing, hives, rapid or weak pulse, hypotension, sweating or an upset stomach with or without nausea, vomiting or diarrhea. I Vasomotor Symptoms: these can occur with or without additional cardiac manifestations. Blood pressure can either increase or decrease, and may be accompanied by ushing or tachycardia. Patients experiencing such reactions may report shortness of breath or tightness in the chest. I Anaphylactoid Reactions: these reactions most commonly include headache, dizziness or lightheadedness. Patients can also experience chills sometimes progressing to rigors, nausea and/or vomiting, back or hip pain, malaise, myalgias and arthralgias. I M M U N E D E F I C I E N C Y F O U N D A T I O N | 2 5 Potential Post-infusion Reactions Post-infusion reactions can occur immediately or as long as 72 hours following the infusion. Common post-infusion reactions may include headache, low-grade fever, nausea, arthralgias and generalized malaise. These reactions are generally managed with over-the-counter analgesics, antihistamines and may require a short course of corticosteroids. Headaches are more frequent in patients who have a history of migraine or cluster headaches. Some patients, particularly those with histories of migraines at other times, may have severe headaches and/or typical migraines up to 72 hours after their infusion. Over-the-counter analgesics are usually effective in treating these headaches, but they sometimes require the addition of oral steroids. The prescriber should always be notied that a reaction has occurred and may wish to change immunoglobulin products or order premedications for future infusions. In addition, all products are produced using techniques to remove or inactivate potentially contaminating viral pathogens. Viral inactivation and removal processes have demonstrated reduction of the potential presence of pathogenic prion agents that have been associated with the development of transmissible spongiform encephalopathy such as variant Creutzfeldt-Jakob disease. These episodes have been noted with increased frequency in patients following rapid infusion protocols or patients with risk factors such as prior thromboembolic events, thrombocytosis, or immobility. Patients with risk factors for thrombotic events should follow a conservative infusion protocol, using a product with a low (5%) concentration, and proceed slowly and cautiously with incremental increases in the rate of infusion to a maximum of 4 ml per kg of body weight per hour. Patients should be given clear instructions regarding what post-infusion symptoms should be reported immediately to their prescriber. I M M U N E D E F I C I E N C Y F O U N D A T I O N | 2 7 I Renal Adverse Events: Potential adverse effects involving the kidneys include acute renal failure, acute tubular necrosis, proximal tubular nephropathy and osmotic nephrosis. Hyperosmolality and the presence of sucrose have been implicated as factors contributing to renal adverse events. Patients who are not adequately hydrated prior to onset of the infusion, who have diabetes mellitus or any pre-existing renal insufciency, those receiving nephrotoxic antibiotics, those who have paraproteinemia, and/or those who are over age 65 are at the greatest risk for these problems. As with patients at greater risk for thrombotic problems, patients with the potential for renal adverse events should be given clear instructions regarding what post-infusion symptoms should be reported immediately to their prescriber. The symptoms may occur during the infusion, but more typically they usually develop within 24 hours of the infusion. A neurologic exam is indicated for these patients to rule our bacterial or viral meningitis. Patients with aseptic meningitis have pleocytosis but no organisms in their cerebrospinal uid. The development of aseptic meningitis is an indication for a change in the immunoglobulin product used for future infusions. Premedication with corticosteroids is also indicated for those with a previous history of infusion related aseptic meningitis. Patients exhibit pulmonary edema, hypoxemia, abnormal left ventricular function, and fever with a typical onset within one to six hours after infusion of the product. Patients at risk include those with a history of atherosclerosis, those who have multiple cardiovascular risk factors, those of advanced age, those with impaired cardiac output, and/or those with known or suspected hyperviscosity or hypercoagulable disorders. This last group of patients include women taking oral contraceptives, especially if they also smoke, and anyone who has had prolonged periods of immobilization. In the United States, the therapy evolved into intramuscular injections and then intravenous infusions. At this time products for subcutaneous infusions are available in concentrations of 10 or 20%. For children or those patients with some physical limitation, someone else can assist with the infusion. Dependent on the volume of drug to be infused, multiple small needles may be used simultaneously. The drug can be administered via a small syringe driver pump or via a manual push. Many studies have demonstrated that patients can tolerate relatively rapid infusions and those patients who deliver their infusions via a manual push can do so in a matter of minutes. For example a dose of 10 grams/week if given with a 20% solution would have a volume of 50 ml. This dose could be split into a twice weekly infusion, using a single needle for each infusion. Deciding how, where and when the infusion occurs may help to minimize time lost from work or school, and allow greater freedom for patients who travel frequently. Patients and/or caregivers will need to be taught the skills necessary to administer their infusions in a safe and aseptic manner. This starts with the nurse rst demonstrating the procedure, then allowing the patient to practice the skill, and nally observing a return demonstration by the patient/caregiver to demonstrate mastery. After the patient is independent, follow up and support are critical in managing issues and/or problems. These might include changing the gauge or length of the needle, a recommendation about using a different site, or changing the rate of the infusion. The important thing to remember is that the vast majority of patients can be successful with this therapy. I M M U N E D E F I C I E N C Y F O U N D A T I O N | 3 1 the most important factors in assuring the success of subcutaneous therapy are teaching and support. A systematic approach to setting up the equipment and drawing up the product, inserting the needle(s), monitoring local effects, discontinuing the infusion, and safely discarding the used equipment and needles needs to be developed. Specific teaching topics can include: I Storage and handling of medication I Traveling with medication, supplies and pumps I Using aseptic technique for drawing up the drug I Priming tubing I Subcutaneous site selection and preparation I Insertion, securing and removal of needles I Checking needle placement to ensure that it has not been inadvertently placed in the intravascular space I Setting up the pump if a pump is going to be used I Anticipating and troubleshooting infusion problems I Discontinuing infusion I Comfort measures and site care I Appropriate waste disposal 3 2 | I D F G U I D E F O R N U R S E S Another important teaching topic is ensuring that the patient understands adverse reactions and/or complications, as well as how to initiate the appropriate action should something untoward occur. The patient must be taught the signs of anaphylaxis and what to do should they occur.
Several such clusters of cases have been described following transplantation symptoms for diabetes buy cordarone 250 mg free shipping, and 1 case was traced to a pet hamster purchased by the donor treatment kidney failure discount cordarone 100mg on-line. Serum specimens from the acute and convalescent phases of illness can be tested for increases in antibody titers by enzyme immunoassays treatment 7th feb cardiff purchase discount cordarone. Because the virus is excreted for long periods of time by rodent hosts symptoms uterine prolapse buy 200mg cordarone, attempts should be made to monitor laboratory and wholesale colonies of mice and hamsters for infection cancer treatment 60 minutes generic cordarone 100mg online. Update: interim guidance for minimizing risk for human lymphocytic choriomeningitis virus infection associated with pet rodents treatment lymphoma cheap cordarone 200 mg free shipping. If appropriate treatment is not administered, fever and paroxysms may occur in a cyclic pattern. Other manifes tations can include nausea, vomiting, diarrhea, cough, tachypnea, arthralgia, myalgia, and abdominal and back pain. Anemia and thrombocytopenia are common, and pallor and jaundice caused by hemolysis may occur. Infection with Plasmodium falciparum, 1 of the 5 Plasmodium species that infect humans, potentially is fatal and most commonly manifests as a febrile nonspecifc illness without localizing signs. People with asplenia who become infected may be at increased risk of more severe illness and death. P knowlesi malaria has been misdiagnosed commonly as the more benign P malariae malaria. Most congenital cases have been caused by P vivax and P falciparum; P malariae and P ovale account for fewer than 20% of such cases. Manifestations can resemble those of neo natal sepsis, including fever and nonspecifc symptoms of poor appetite, irritability, and lethargy. The 5 species that frequently infect humans are P falciparum, P vivax, P ovale, P malariae, and P knowlesi. These conditions have resulted in recent cases in travelers to areas such as Jamaica, the Dominican Republic, and the Bahamas. Uncommon modes of malaria transmission are congenital, through transfusions, or through the use of contaminated needles or syringes. P falciparum malaria is prevalent in Africa, Papua New Guinea, and on the island of Hispaniola (Haiti and the Dominican Republic). P vivax and P falciparum species are the most common malaria species in southern and Southeast Asia, Oceania, and South America. P ovale malaria occurs most often in West Africa but has been reported in other areas. Relapses may occur in P vivax and P ovale malaria because of a persistent hepatic (hypnozoite) stage of infection. The spread of chloroquine-resistant P falciparum strains throughout the world is of increasing concern. In addition, resistance to other antimalarial drugs also is occurring in many areas where the drugs are used widely. P falciparum resistance to sulfadoxine pyrimethamine is common throughout Africa, mefoquine resistance has been docu mented in Burma (Myanmar), Laos, Thailand, Cambodia, China, and Vietnam, and emerging resistance to artemisinins has been observed at the Cambodia-Thailand border. Chloroquine-resistant P vivax has been reported in Indonesia, Papua New Guinea, the Solomon Islands, Myanmar, India, and Guyana. More than 80% of cases diagnosed in the United States occur in people who have onset of symptoms after their return to the United States. The thick flm allows for concentration of the blood to fnd parasites that may be pres ent in small numbers, whereas the thin flm is most useful for species identifcation and determination of the degree of parasitemia (the percentage of erythrocytes harboring parasites). If initial blood smears test negative for Plasmodium species but malaria remains a possibility, the smear should be repeated every 12 to 24 hours during a 72-hour period. Confrmation and identifcation of the species of malaria parasites on the blood smear is important in guiding therapy. Both positive and negative rapid diagnostic test results should be confrmed by microscopic examination, because low-level parasitemia may not be detected, false-positive results occur, and mixed infections may not be detected accurately. Also, information about the sensitivity of rapid diagnostic tests for the 2 less common species of malaria, P ovale and P malariae, is limited. More informa tion about rapid diagnostic testing for malaria is available at Patients with severe malaria require intensive care and parenteral treatment until the parasite density decreases to less than 1% and they are able to tolerate oral therapy. For example, if there is concern about individual tolerance with mefoquine, then prophylaxis can be started 3 weeks before travel. Most adverse events will occur during the frst 3 doses, and if the individual does not tolerate mefoquine, then there still is time to prescribe alternative therapy before travel. Travelers to areas where chloroquine-resistant P falciparum exists should take atovaquone-proguanil, doxycycline, or mefoquine. Adverse reactions that can occur include gastrointestinal tract disturbance, headache, dizziness, blurred vision, insomnia, and pruritus, but these generally are mild and do not require discontinuation of the drug. Drugs for the prevention of malaria currently available in the United States include chloroquine, mefoquine, doxycycline, atovaquone-proguanil, and primaquine. Atovaquone-proguanil is taken daily, starting 1 day before exposure and continuing for the duration of exposure and for 1 week after departure from the area with endemic malaria. Travelers taking doxycycline should be advised of the need for strict adherence to daily dosing; the advisability of always taking the drug on a full stomach; and the possible adverse effects, including diarrhea, photosensitivity, and increased risk of monilial vaginitis. Use of doxycycline should be avoided for pregnant women and for children younger than 8 years of age because of the risk of dental staining (see Antimicrobial Agents and Related Therapy, Tetracyclines, p 801). However, parents should be advised not to travel to countries with endemic malaria with children weighing less than 5 kg or younger than 6 weeks of age because of the risks associated with infection (septicemia or malaria) in young infants. The most com mon central nervous system abnormalities associated with mefoquine are dizziness, headache, insomnia, and disturbing dreams. Other adverse events that occur with prophylactic doses include gastrointestinal tract disturbances, headache, depression, and anxiety disor ders. Caution should be advised for travelers involved in tasks requiring fne motor coordination and spatial discrimination. Patients in whom mefoquine prophylaxis fails should be monitored closely if they are treated with quini dine or quinine sulfate, because either drug may exacerbate known adverse effects of mefoquine. The artemisinins are derived from the leaves of the Artemisia annua plant used to treat malaria. Primaquine is recommended for prophylaxis in areas with predominantly P vivax malaria. Primary primaquine prophylaxis should begin 1 to 2 days before departure to the area with risk of malaria and should be continued once a day while in the area with risk of malaria and daily for 7 days after leaving the area. For these reasons and because no chemoprophylactic regimen completely is effec tive, women who are pregnant or likely to become pregnant should try to avoid travel to areas where they could contract malaria. Pregnancy and lactation, therefore, are not contraindica tions for malaria prophylaxis with chloroquine. Consequently, mefoquine is the drug of choice for prophylactic use for women who are pregnant or likely to become pregnant when exposure to chloroquine-resistant P falciparum is unavoidable. Lactating mothers of infants weighing more than 5 kg may also use atovaquone-proguanil or mefoquine for prophylaxis when exposure to chloro quine-resistant P falciparum is unavoidable. Travelers to malaria-endemic settings should seek medical attention immediately if they develop fever. Malaria can be treated effectively early in the course of disease, but delay of appropriate treatment can have serious or even fatal consequences. If they are diagnosed with malaria while traveling, they will have a medicine that will not interact with their other medications, is of good quality, and is not depleting local resources. Travelers taking atovaquone-proguanil as their antimalarial drug regimen should not take atovaquone-proguanil for treatment and should use an alternative antimalarial regi men recommended by a travel medicine expert. Travelers should be advised that any fever or infuenza-like illness that develops within 3 months of departure from an area with endemic malaria requires immediate medical evaluation, including blood flms to rule out malaria. To be effective, most repellents require frequent reappli cations (see Prevention of Mosquitoborne Infections, p 209, for recommendations regarding prevention of mosquitoborne infections and use of insect repellents). In temperate areas, the peak incidence of infection usually occurs during late winter and spring. The childhood and adolescent immunization program in the United States has resulted in a greater than 99% decrease in the reported incidence of measles and interruption of endemic disease transmission since measles vaccine frst was licensed in 1963. In 2000, an independent panel of internationally recognized experts reviewed available data and unanimously agreed that measles no longer was endemic (continuous, year-round transmission) in the United States. Cases are considered international importations if the rash onset occurs within 21 days after entering the United States. Seventy-two of the cases were direct importations from 20 to 22 countries, and 17 outbreaks (3 or more cases) occurred. The majority (approximately 85%) of cases were in people who were unimmunized or had unknown immunization status, including 27 cases in infants younger than 12 months of age, some of whom had traveled abroad. Although waning immunity after immunization may be a factor in some cases, most cases of measles in previously immunized children seem to occur in people in whom response to the vaccine was inadequate (ie, primary vaccine failures). In family studies, the average interval between appearance of rash in the index case and subsequent cases is 14 days, with a range of 7 to 21 days. The simplest method of establishing the diagnosis of measles is testing for IgM antibody on a single serum speci men obtained during the frst encounter with a person suspected of having disease. If the result is negative for measles IgM and the patient has a generalized rash lasting more than 72 hours, a second serum specimen should be obtained, and the measles IgM test should be repeated. Therefore, a negative IgM test should not be used to rule out the diagnosis in immunized people. All cases of suspected measles should be reported immediately to the local or state health department without waiting for results of diagnostic tests. Measles virus is susceptible in vitro to ribavirin, which has been given by the intravenous and aerosol routes to treat severely affected and immunocompromised children with measles. Vitamin A treatment of children with measles in developing countries has been associated with decreased morbidity and mortality rates. Immunization is the intervention of choice for control of measles outbreaks in schools and child care centers. Measles containing vaccines can be given simultaneously with other immunizations in a separate syringe at a separate site (see Simultaneous Administration of Multiple Vaccines, p 33). Since 1979, an improved stabilizer has been added to the vaccine that makes it more resistant to heat inactivation. Delays in administering the frst dose contributed to large outbreaks in the United States from 1989 to 1991. The second dose is recommended routinely at school entry (ie, 4 through 6 years of age) but can be given at any earlier age (eg, during an outbreak or before interna tional travel), provided the interval between the frst and second doses is at least 28 days. If a child receives a dose of measles vaccine before 12 months of age, this dose is not considered valid, and 2 doses are required beginning at 12 through 15 months of age and separated by at least 4 weeks. However, the recommended minimal interval between varicella vaccine doses is 90 days. The period of risk for febrile seizures is from 5 to 12 days following receipt of the vac cine. Pediatricians should discuss risks and benefts of the vaccine choices with the par ents or caregivers. Doses received prior to the frst birthday should not count toward the recommended 2-dose series. Children 12 months of age or older who have received 1 dose and are traveling to areas where measles is endemic or epidemic should receive their second dose before departure, pro vided the interval between doses is 28 days or more. Because the incidence of encephalitis or encephalopathy after measles immunization in the United States is lower than the observed incidence of encephalitis of unknown cause, some or most of the rare reported severe neurologic disorders may be related coincidentally, rather than causally, to measles immunization. Reactions have been attributed to trace amounts of neomycin or gelatin or some other component in the vaccine formulation. Measles vaccine is produced in chicken embryo cell culture and does not contain signifcant amounts of egg white (ovalbumin) cross-reacting proteins. People with allergies to chickens or feathers are not at increased risk of reaction to the vaccine. People who have had a signifcant hypersensitivity reaction after the frst dose of measles vaccine should: (1) be tested for measles immunity, and if immune, should not be given a second dose; or (2) receive evaluation and possible skin testing before receiving a second dose. People who have experienced anaphylactic reactions to gelatin or topically or systemi cally administered neomycin should receive measles vaccine only in settings where such reactions can be managed and after consultation with an allergist or immunologist. Most often, however, neomycin allergy manifests as contact dermatitis, which is not a contrain dication to receiving measles vaccine. The decision to immunize these children should be based on assessment of immunity after the frst dose and the benefts of protection against measles, mumps, and rubella in comparison with the risks of recurrence of thrombocytopenia after immunization. Management of immunodefcient and immunosuppressed patients exposed to measles can be facilitated by previous knowledge of their immune status. If possible, chil dren should receive measles vaccine prior to initiating treatment with bio logical response modifers, such as tumor necrosis factor antagonists. For patients who have received high doses of corticosteroids (2 mg/kg or greater than 20 mg/day of prednisone or its equivalent) for 14 days or more and who otherwise are not immunocompromised, the recommended interval before immunization is at least 1 month (see Immunocompromised Children, p 74).
Discount 250 mg cordarone fast delivery. Osteoporosis symptoms causes and other risk factors.