James I. Cohen, MD, PhD, FACS
- Professor, Department of Otolaryngology/Head and Neck Surgery
- Chief Otolaryngology/Assistant Chief Surgery, Portland VA
- Medical Center
- Oregon Health and Science University
- Portland, Oregon
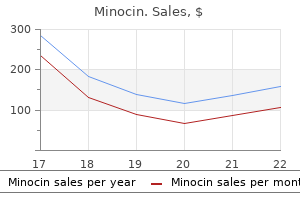
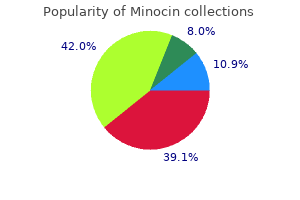
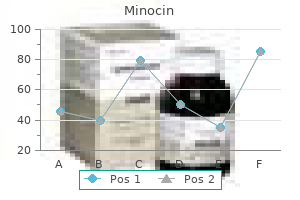
To improve comparability of the results between the States the estimation of the performance indicators was restricted oral antibiotics for acne philippines buy generic minocin 50 mg on-line the age range 30-59 years antibiotic resistance vibrio cholerae cheap minocin 50 mg overnight delivery, which was common bacteria 365 days plague inc order minocin now all antibiotic resistance cases purchase minocin in united states online. Further assessment (colposcopy referral) rates Positive screening tests require further assessment antibiotics for uti webmd purchase 50 mg minocin amex. In the 30-59 year age group (excluding Hungary antibiotic mnemonics discount 50 mg minocin, where colposcopy is substantially part of the primary screening visit) 2. Further assessment participation rates For areas providing information, the European mean for the colposcopy participation rates for all ages was 76. It must be taken into account that in some countries the detection rates are underestimated due incomplete registration of the histology reports for the colposcopies performed outside the programme. We received quantitative performance data from 2 out of 4 non-population-based programmes (Czech Republic and Latvia), while, out of 19 member states with population based programmes, 16 provided quantitative data on invitation and examinations (no data from Austria, Cyprus and Denmark) and 15 provided quantitative data on test and assessment results (no data from Austria, Cyprus, Denmark and Portugal) also. Coverage by invitation and examination Data about screening invitations and examinations have been provided by 18 (78. Among responders, three countries (Czech Republic, Latvia and Lithuania) had not implemented an active invitation system, while the remaining 15 were inviting their entire target population at regular intervals specified by their screening protocol. The expected cost-effectiveness ratio is dependent on several factors, including background risk, screening method, organisation of the programme, resources in health care and also on the age range targeted by the programme. In addition, as also methods using non-invasive faecal tests for primary screening will require colonoscopy assessments of positive subjects, issues related colonoscopy capacity are also influencing the choice of the method, as well as of the target age range, in different jurisdictions. The annual target population was calculated by dividing the total population in the age range divided by the screening interval. The variability across member states for both indicators is fairly wide: the 10-90 percentile range is 8. The examination coverage in the 50-74 years age group across different member states is also shown in figure 4. It should be considered that these latter estimates could only be derived over a uniform target population. These estimates did not take into account that in many countries the actual target age group was narrower. The estimates presented do not take into account (relevant data were not collected) the impact of policies stipulating the exclusion from invitation of ineligible subjects in the target population. However, exclusion criteria are not standardised across countries, they are highly dependent on organisational policy decisions and their adoption has been criticised, give there are often based on inaccurate information. A recent review of the 29 measures adopted estimate participation concluded that the validity of international comparisons could be improved by reporting sex-, age-, screening test and screening 21 history specific participation rates, without taking into account exclusion criteria. Coverage by examination is reflecting the participation rates, which are influenced by gender and screening protocol; as expected, women are showing a higher coverage than men in all countries using faecal test, while the opposite is true in those countries implementing endoscopy screening. Indeed, the screening programme in Austria is covering about 4% of the 50-74 year Austrian population, the programme in Denmark, targeting 1. So the reported figures for invitation coverage are likely be representative of the 2012-2104 situations. Some countries implementing the programme at the regional level have not yet completed the rollout phase. In Sweden the programme was initiated only in the Stockholm region, making up 20% of the Swedish population aged 60 69 years and in the other parts of the country a large-scale randomized screening trial on novel screening strategies is on-going (ClinicalTrials. Other countries are implementing their programme following a stepwise approach, designed achieve full-coverage over a pre-specified time interval. The duration of the rollout phase, as well as the timing of the inclusion of the targeted birth cohorts, has been determined based on resource implementation plans (The Netherlands), or on the design requirements of the planned randomised health services evaluation (Finland and Poland). When assuming the actual population targeted by the programmes as the reference for estimating programme coverage, the estimated proportion of subjects invited increases from 36. Participation rate is indeed defined as the percentage of subjects screened in a particular year out of the total number of those who had received a personal invitation in that year. On the other hand, from a public health point of view as a certain proportion of non-responders will attend at least once over repeated invitations, a higher proportion of subjects in the target population will benefit some extent from the protective effects of screening protocols using tests be repeated at regular intervals. Such strategy results in substantial increase in the population coverage, similar among men and women. Completeness of information Data collection aimed at describing by appropriate summary indicators the entire process of care, from invitation screening examination, further assessment, and final diagnosis. The extent which this information has been made available by the Member States or the regions is illustrated in Table 4. Data about the different phases of the screening process, including the information about attendance (tests returned), test results compliance with the referral for colonoscopy assessment and the availability of the histology result of the subjects having a positive primary screening test, are available for 15 (no data could be provided by Austria, Cyprus, Denmark and Portugal) out of 19 countries having implemented a population-based programme and for 2 (Czech Republic and Latvia) of the 4 countries having implemented non-population-based screening. Stratified data by gender and screening history are presented in the tables as follows: by gender tables 4. Positive screening test results Rates of positive screening test results reflect the cut-off level chosen in each Member State for the adopted test. It should be considered that this proportion is also reflecting the programmes policies defining the management of these subjects who are usually requested repeat the test: the reported figures are referring the proportion of subjects who did not repeat (refusers and not yet re-invited). Also, the proportion of inadequate sample is higher at the first screening as compared subsequent screening rounds. Follow-up colonoscopy participation rates Compliance with assessment colonoscopy referral among subjects with a positive screening test is around 80% in most countries independent of the primary screening method. Compliance was below 50% in the only non-population-based programme reporting these information, while the average for population-based programmes was 73. Follow-up colonoscopy and screening colonoscopy completion rates Information on completion rate of assessment examinations is incomplete in several countries. Available data would suggest, however, that the quality of the examinations is generally satisfactory, with several programmes reporting completion rates over 90%. As 32 expected, completion rates tend be lower among women than among men, and this is true even when colonoscopy is offered as primary screening test. Such disparities also contribute the observed variations in the diagnostic performances of the tests. Cross-countries comparisons, even among those using the same type of tests are therefore difficult. We have also presented detailed data stratified by gender, age and screening history, whenever available. Direct comparisons within these strata may offer more relevant indications compare the performance of different screening protocols. Detection rates of colorectal cancers Colorectal cancer detection rates ranged between 0. The same trend can be observed also when restricting the analysis the 60 69 year age group, targeted by most programmes, reduce variability related the age distribution of the screened population. The Council Recommendation also comprises specific items relevant for organisational components and systematic quality assurance of the population-based cancer screening for breast, cervical and colorectal cancers and efforts aimed at achieving and maintaining an appropriate balance between benefit and harm of screening in these programmes. As recommended by the Council, the current, second implementation report measured the availability of screening registries and databases, and collected and reported quantitative information on the performance and quality indicators of screening programmes using the screening registries as the main information source. Qualitative information relevant for validation of the screening registry based data as well as information on organizational aspects of the programmes was also collected. The size of the target population for cervical cancer screening is much bigger (106. The accomplishments of the member states in implementing colorectal cancer screening within the relatively short period of time are remarkable. The increase in colorectal cancer screening has been particularly spectacular, because prior 2003 no Member State had implemented a full-scale colorectal cancer screening programme, and their planning, piloting and rollout full implementation began mostly after the Council recommendations. The population coverage of one or more of the cancer screening programmes is rather low or even very low in many of the Member States, indicating a low rate of acceptance by the population, and possibly also inadequate adherence by the policy-makers and medical professionals the quality assurance requirements. Low coverage also indicates the presence of health inequities and social inequalities. In many countries, appropriate monitoring of screening activities was not yet in place. The monitoring databases are necessary not only for accountability of cancer screening but also for evaluating the screening outcomes and the potential adverse effects and harms. Furthermore, some of the key performance indicators, such as detection rates and positive predictive values for histologically confirmed findings indicated wide variations between the national programmes and between regional programmes (with variation also possible within programmes, i. In interpreting these variations, the different prevalence or underlying incidence of the condition must be taken into account. Moreover, although we standardized data collection and asked for the numerical components of the indicators. The impact of these variations upon the overall effectiveness and balance of benefit and harm deserves further investigation. These services reach very large segments of the population provide highly specialized multidisciplinary services and integrate a broad range of health care providers, regulatory agencies and other institutions. Strengths of the study Our call the data providers had a high response rate in the Member States and information was received from each population-based programme. Respondents had a formal status through the ministries of health or other health authorities of the Member States, so that the authorities could check the contents whenever needed. The official data sources (including screening registries and their statistics; national quality manuals and guidelines; legislation) were used, and the questionnaire data collection process included further documentation of the data sources by each country in order for the authors verify these responses. Performance data from official screening registries provided further information on the current implementation status, for example information on coverage and detection rates in the programmes, using standard definitions from the European guidelines as much as possible. These indicators contribute the evaluation of the national programmes and enable comparisons among countries and regional programmes. Limitations Although the European Guidelines on cancer screening and the activity of the European Cancer Screening Network contributed homogeneity, the screening protocols adopted by Member States and the organisation of data collection and evaluation may differ and make some comparisons difficult. However, as it has been illustrated in the Methods section, this 36 report is based on structured and standardised data collection and on detailed documentation, so limit this problem. The present report does not substantially include opportunistic activity, which is not recommended by the European Council (2003). The size of opportunistic activity is particularly relevant for cervical screening. Screening data on the overall number of women tested in the index year, including those screened on their own initiative, is available for countries that use an integrated approach. However, registered data or interview surveys show that opportunistic activity can be very large also in countries that invite all women. For breast cancer screening no quantitative data were reported by the three countries having implemented non-population based screening only. For colorectal cancer screening quantitative data were reported by two out of four countries having implemented only non population based screening at the time of data collection. For both sites, opportunistic testing is ongoing also in those countries having introduced population based programmes. Quantitative data on such activity, generally derived by population health surveys, are limited, often showing a marginal contribution of such activity the population coverage. Testing of the population outside the target age groups and intervals of population based programmes, although common, is poorly documented, and is generally not subjected the systematic quality assurance recommended for screening programmes. Related over diagnosis and overtreatment of regressive cervical precancerous lesions, and overly frequent opportunistic testing all contribute increased health care costs. Opportunistic testing brings social inequalities when the more affluent can more readily obtain the benefits of testing than the less affluent. One reason for the choice collect data substantially only on the activity of population based programmes is precisely the fact that organised screening only is recommended by the European Council, because of its many and well documented advantages (see Introduction). Another reason is that in many situations data on the opportunistic activity are simply not available because they are not registered. Nevertheless the existence of opportunistic activity must be kept in mind: o When interpreting examination coverage. The reported coverage, that considers only screening after invitation, is plausibly, in some case, much lower than the proportion of women who was tested during a screening round. Costs are usually lower in presence of a population based screening but this requires a reduction of the opportunistic activity Successful planning, preparation and completion of the nationwide implementation process may require a decade or longer. Three additional current Member States were running or establishing population-based programmes in 2016. Nationwide rollout of population-based screening is currently complete in 22 of these Member States with an approximate target population of 60 million women aged 50-69 years. It is encouraging note that pilot or demonstration projects undertaken in preparation for nationwide screening, have been completed or are ongoing in two of the countries without population-based programmes at present (Bulgaria and Romania). In addition there was very wide non-population-based activities meant for cancer screening purposes, utilizing often opportunistic, non-regulated policies and protocols. In 2007, four years after the adoption of the Council recommendation, only 15 Member States, representing less than half of the potential target population, had population-based 11 screening activities for cervical cancer, whereas in 2016 population-based screening for cervical cancer is provided or planned in 22 countries targeting nearly three fourth of the nearly 106 million target population. Colorectal cancer screening the first report on the implementation status showed that 19 Member States were running, 11 piloting or planning colorectal cancer screening programmes in 2007 though none of them had full-scale implementation of population-based programmes, i. The number of Member States reported 38 have colorectal cancer screening programmes in an international survey conducted in 2003 32 and 2004 was much smaller. National or regional programmes were reported in the survey only for the Czech Republic, Italy and Poland, and pilot projects were found in France, Italy, Spain and the United Kingdom. The current status of colorectal cancer screening in Europe shows 23 countries having the programme either already implemented or in the planning phase, of which 11 countries have rollout completed either nationwide or regionally. More than 110 million women and men are being targeted by these population-based programmes. On the other hand, some of the Member States were not able deliver a minimum set of data that is considered essential for directing quality assurance activities. Continuing European monitoring of these essential parameters would certainly improve the extent and quality of screening data, stimulate networking and enhance screening effectiveness in the Union. A coordinated strategy for delivering services and collecting information will further improve the planning and delivery of screening services.
EcF and since E and EcF are mutually exclusive we have that c P(F) = P(E) + P(E F)? Because the 253 events that persons i and j have the same birthday are not mutually exclusive virus protection generic 50 mg minocin with amex. Consequently medication for uti bladder spasm order minocin 50mg with visa, the probability that a randomly chosen accountant will have a salary in this range is at least 3/4 antibiotic powder minocin 50mg without prescription. Hence antibiotics and probiotics purchase minocin 50 mg without prescription, the probability that a randomly chosen accountant will have a salary that exceeds this amount is at most 4/13 bacteria jacuzzi purchase discount minocin. P(D1D2) P(D2|D1) = P(D1) P(D1D2|A)P(A) + P(D1D2|B)P(B) = P(D1|A)P(A) + P(D1|B)(P(B) antibiotics stomach ache generic 50 mg minocin with visa. Then P A be executed | jailer says B = P{A executed, B}/P P1/3 = P{B|A exec. Since brown is dominant over blue the fact that you have blue eyes means that both your parents have one brown and one blue gene. Now, imagine that the teams continue play even after the series winner is decided. Le t 1 be the card of lowest value, 2 be the card of next higher value, and 3 be the card of highest value. Le t C be the event that the household is from California and let O be the event that it earns over 250, 000. The probability that a given radio tube will last less than 150 hours is 0 f (x)dx = 5 1? Wit h p(i, j) = P(N1 = i, N2 = j) p(1, 1) = (3/5)(2/4) = 3/10 p(1, 2) = (3/5)(2/4)(2/3) = 2/10 p(1, 3) = (3/5)(2/4)(1/3) = 1/10 p(2, 1) = (2/5)(3/4)(2/3) = 2/10 p(2, 2) = (2/5)(3/4)(1/3) = 1/10 p(3, 1) = (2/5)(1/4) = 1/10 p(i, j) = oth e rwis 11. The expected score of a meteorologist who says that it will rain with probability p is? Suppose the white balls are arbitrarily numbered before the selection and let 1 if white ball number i is selected, Yi = 0 oth erwise. Independence is needed for i i i the variance but not for the expectation (since the expected value of a sum is always the sum of the expected values but the corresponding result for variances requires independence). Clearly, the maximum is obtained when p1 = 1/2 the largest possible value of p1 since p3 = p1 (andp2 = 0, p3 = 1/2) and the minimum when p1 = 0(andp2 = 1, p3 = 0). If N1 is large, then a large number of trials result in outcome1, implying that there are fewer possible trials that can result outcome 2. From 0 this it is easy see that nth derivative evaluated at t = 0isequalto1/(n + 1) = E[Xn]. X, the number of failures, in n independent trials each of which is a success with probability p. The result follows by noting that X and Y are both binomial with respective parameters (n p) and (n 1? Since the sum of independent Poisson random variables remains a Poisson random variable, it has the same distribution as the sum of n independent Poisson random variables with mean? Using that 9S2/4 and 4S2/2 are chi squares with respective degrees of freedom 9 and 1 2 4showsthatS2/(2S2) is an F random variable with degrees of freedom 9 and 4. X, the number of men that rarely eat breakfast is approximately a normal random variable with mean 300(. Using these estimates the length of the tower, call it T, is estimated as follows: T = X tan(? Now choose the total sample size n (= 30 + additional sample v size) be such that 2z? In all cases the desired probability is obtained by integrating this density from p equal 0 p equal. This has be done numerically as the above does not have a closed form integral. If the selection was random, then the data would constitute a sample of size 25 from a normal population with mean 32 and standard deviation 4. The null hypothesis should be that the mean time is greater than or equal 10 minutes. Thus the hypothesis is rejected at neither the 1 nor the 5 percent level of signi? Testing the null hypothesis that the mean number of cavities is at the least 3 gives p-value = P3{X? With T27 being a t-random variable with 27 degrees of freedom v p-value = P{|T27|? The p-value of the test of the null hypothesis that the mean temperature is equal 98. Us ing the Fisher-Irwin conditional test, the p-value is twice the probability that a hypergeometric random variable X, equal the number of red balls chosen when a sample of 83 balls is randomly chosen from a collection of 84 red and 72 blue balls, is at most 44. By the normal approximation, the binomial it follows that Y is approximately normally distributed and so (a) follows. The scientist should try match her samples, so that for each smoker there is a nonsmoker of roughly the same age. No because the researcher will only be considering stocks that have been around for the past 20 years, and is thus ignoring those that were in play 20 years ago but have since gone bust. Taking logsandletting time be the independent variable yields, upon running Program 9-2, the estimates log a =. Thus, at the 5% level we would accept when the sign test and reject when the using the signed rank test. The probability that the next subgroup falls outside v v v is approximately P{X > 14 + 6/ 5}=P{Z >(6/ 52. On average, it will take a geometric distributed number of subgroups with mean 1/. Thus if n are produced on a day then the number of defects should be within np sqr{np(1? In either case this is equal the total time on test divided by the number of observed failures. So, the permutation before the interchange is equally likely be either P1 = 1, 2, 3 or P2 = 2, 1, 3. The value of the test statistic T, equal the sum of the group 1 lifetimes, is T = 1389. It appears as a single red spot or many scattered red spots on the white of the eye. The conjunctiva is the skin of the eye, and it is a clear layer of skin that covers the white of the eye and the inner eyelids. A subconjunctival hemorrhage is usually painless, does not affect your vision, and heals on its own. Subconjunctival hemorrhage occurs when blood vessels in the conjunctiva break causing blood leak. Common causes of this are eye trauma, coughing, sneezing, straining, or any activity that raises blood pressure in the veins. This happens more frequently if a person is taking blood thinners like aspirin or Coumadin. You may not even know that it is there until you look in the mirror or someone else points it out. Kellogg Eye Center Subconjunctival Hemorrhage 1 How is subconjunctival hemorrhage treated? If your eye is irritated at all, you can use artificial tears that you can buy over-the-counter. What is Sub-conjunctival Haemorrhage the white part of the eye (known as the sclera) is covered by a transparent membrane called the conjunctiva. A sub-conj haemorrhage occurs when these tiny blood vessels leak, causing a small amount of blood gather between the sclera and conjunctiva. Symptoms the eye will look bloodshot and you may have a feeling of tightness in the affected eye. The causes of sub-conjunctival haemorrhage Practically all sub-conj haemorrhages occur for no apparent reason. Diabetes or high blood pressure may make you slightly more likely get a sub-conj haemorrhage 3. Generally, patients with a sub conj haemorrhage do not need be seen in the Eye Hospital clinic. How contact us If you have any questions concerning your eye condition or treatment, please do not hesitate contact the eye nurses answerphone on: 01865 231099 One of the nurses will call you back. This Other potential causes include injury bleeding is caused by the leaking of a the eye or rubbing the eye forcefully. It may be flat or check your vision, examine your eye occasionally slightly raised above the with a slit lamp, and check your blood surface of the eye. Sometimes, this condition usually does not require you might not notice it until somebody any treatment and will settle by itself draws your attention it. Subconjunctival haemorrhages are very common because the blood Please note: if you have repeated vessels in the conjunctiva are very subconjunctival haemorrhages, you fragile and can easily bleed a little. Disch arge Iritis Injected Small, N ormal, T urgid, N ormal around cornea fixed, K Ps deep irregular A cute glaucom a Entire eye red F ixed, H az y Sh allow H igh dilated, oval C onjunctivitis F ollicles Purulentdisch arge Papillae C h emosis R edness S ubconjunctivalH aem orrh age. Features such as signifcant pain, photophobia, reduced visual acuity and a unilateral presentation are red fags that a sight-threatening condition may be present. In the absence of specialised eye examination equipment, such as a slit lamp, General Practitioners must rely on identifying these key features know which patients require referral an Ophthalmologist for further assessment. Is it conjunctivitis or is it something more Iritis is also known as anterior uveitis; posterior uveitis is serious? However, red eye can also be presentation, usually associated with autoimmune a feature of a more serious eye condition, in which a delay in disease. In addition, the inappropriate use of antibacterial eye is not always a feature topical eye preparations contributes antimicrobial 6. The patient history will usually identify a penetrating eye injury Most general practice clinics will not have access specialised or chemical burn the eye, but further assessment may be equipment for eye examination. In History and eye examination general, a patient with a unilateral presentation of a red eye the most important fndings in a patient with a red eye are the suggests a more serious cause than a bilateral presentation. Acute angle closure glaucoma occurs when there is an Duration, nature and onset of symptoms obstruction drainage of aqueous humour from the Dull, stabbing, throbbing or gritty pain? Microbial keratitis is usually precipitated by a change normal corneal epithelial Past ocular history health, caused by a factor such as trauma, contact lens Previous episodes? Infammation anterior chamber chamber (iridocorneal angle) afects (conjunctivitis) causes vascular the drainage rate of aqueous humour dilatation and can produce from the anterior chamber into the signifcant oedema of this tissue trabecular meshwork; a narrow or (chemosis). Choroid A vascular layer between the sclera Iris A thin, opaque (coloured), circular and retina that provides oxygen and structure that controls the size of the nutrition the retina pupil and the amount of light that reaches the retina Ciliary body the circumferential tissue, anterior the retina, composed of ciliary Lens A biconvex structure behind the muscle and ciliary processes that iris that helps refract light change the shape of the lens accurately focus on the retina adjust focus a process called accommodation. The ciliary Limbus the border between the sclera and processes also produce aqueous the cornea humour. Examination and assessment Measure pupillary response/light refexes the extent of the eye examination should be based on Examine the cornea; is it clear or opaque/hazy? The patient should wear their corrective injury distance glasses, if they have them. If the patient has discharge Examine the eyelids in their eye(s), ask them blink several times before checking Is lid position normal? Examine the eye: Assess the extent, location and nature of the redness of the eye(s) Assessing the cornea with fuorescein dye: Fluorescein is an the pattern of injection (redness) should also be orange dye that fuoresces green under blue light. It dissolves noted: conjunctival injection (Figure 1) appears as into the tear flm creating a homogenous green glow across a difuse area of dilated blood vessels, injection in a the ocular surface, with increased intensity where the tears accumulate on the lower lid margin. Any area of epithelial ring-like pattern around the cornea is termed ciliary defect will stain brightly, allowing detection of corneal injection (Figure 2) and usually indicates intraocular infammation abrasions, ulcers and foreign bodies. Figure 1: Conjunctival injection showing a difuse pattern Figure 2: Ciliary injection showing a ring-like pattern of of dilated blood vessels. Photo kindly supplied by Dr Logan Mitchell, dilated blood vessels around the cornea, which indicates Department of Medicine, University of Otago. Photo kindly supplied by Dr Logan Mitchell, Department of Medicine, University of Otago. Instil the dye by either touching across the globe, ideally using an intravenous giving set. Check a fluorescein strip the inside of the lower eyelid, or the pH of the tear flm using litmus paper two three minutes applying a drop of fluorescein dye eye drops; ask the after each bag of fuid and repeat until the pH measures 7 8 patient blink distribute the dye. Tetanus status should be determined, a hard shield taped Refer serious causes of red eye over the eye (without exerting pressure on the globe), and the patient instructed not eat or drink in preparation for Stop! A penetrating injury may be obvious in the Patients with the following features should be case of a grossly misshapen globe or a full-thickness corneal referred urgently (same day) for ophthalmological or scleral laceration with prolapse of intraocular contents. Patients with an injury caused by a high Reduced visual acuity (after correcting for refractive velocity object. Many patients with red eye may have ambiguous features and require a slit-lamp examination be certain of a diagnosis. If there is any suspicion of a serious cause then discussion with an Ophthalmologist is recommended. A triage assessment by an Optometrist may also be useful, especially in remote locations. Refer urgently for an ophthalmological assessment if the patient is suspected have acute angle closure glaucoma, iritis, scleritis, infectious/infammatory keratitis or a penetrating eye injury. Patients with a serious chemical eye injury also require Figure 3: Acute glaucoma showing hazy cornea, indistinct urgent referral but the frst priority is irrigation of the ocular iris and fxed, mid-dilated pupil. Photo kindly supplied by Dr Logan surface: topical anaesthetic should be applied, the eyelids held Mitchell, Department of Medicine, University of Otago. In severe cases, a a tonometer (to measure the intraocular pressure), digitally level of purulent exudate within the anterior chamber may be palpating the globe behind closed eyelids and comparing seen (a hypopyon). Refer an Ophthalmologist for treatment, globe firmness provides useful information. While Iritis (anterior uveitis) is often very painful due ciliary waiting, the patient should lie fat with their face up, without a muscle spasm.
Prostate Cancer Age-Adjusted Mortality Rates* by Jurisdiction and Race antibiotic video buy minocin 50mg low price, Maryland medication for uti relief discount minocin express, 2014 Race Jurisdiction Total Whites Blacks Other Maryland 19 bacteria en el estomago purchase minocin online pills. Prostate Cancer Age-Adjusted Incidence Rates* by Jurisdiction and Race antibiotics used for cellulitis order cheap minocin on-line, Maryland infection of the bone order 50mg minocin otc, 2010-2014 Race Jurisdiction Total Whites Blacks Other Maryland 125 antibiotics respiratory infection purchase minocin 50 mg without a prescription. Prostate Cancer Age-Adjusted Mortality Rates* by Jurisdiction and Race, Maryland, 2010-2014 Race Jurisdiction Total Whites Blacks Other Maryland 20. Maryland area-specific rates with 95% confidence intervals are presented in Appendix E, Table 5. Maryland area-specific rates with 95% confidence intervals are presented in Appendix E, Table 13. Oral Cancer Incidence (New Cases) In 2014, a total of 731 cases of cancer of the oral cavity and pharynx (called oral cancer) were reported in Maryland. Maryland had the 37 highest oral cancer mortality rate among the states and the District of Columbia for the period 2010-2014. Oral cancer mortality rates have increased from 2010 2014, with a rate increase of 0. Source: Maryland Cancer Registry 80 Mortality Trends by Race Over the 5-year period from 2010 2014, oral cancer mortality rates decreased at a rate of 0. From 2010 2014, the proportion of oral cancers reported as unstaged gradually decreased. Source: Maryland Cancer Registry 81 Oral Cancer Screening There is no current Healthy People 2020 target for oral cancer screening. The Maryland 2020 objective from the Comprehensive Cancer Control Plan is increase 26. Oral Cancer Age-Adjusted Incidence Rates* by Jurisdiction, Gender, and Race, Maryland, 2014 Gender Race Jurisdiction Total Males Females Whites Blacks Other Maryland 10. Oral Cancer Age-Adjusted Mortality Rates* by Jurisdiction, Gender, and Race, Maryland, 2014 Gender Race Jurisdiction Total Males Females Whites Blacks Other Maryland 2. Oral Cancer Age-Adjusted Incidence Rates* by Jurisdiction, Gender, and Race, Maryland, 2010-2014 Gender Race Jurisdiction Total Males Females Whites Blacks Other Maryland 10. Oral Cancer Age-Adjusted Mortality Rates* by Jurisdiction, Gender, and Race, Maryland, 2010-2014 Gender Race Jurisdiction Total Males Females Whites Blacks Other Maryland 2. Maryland area-specific rates with 95% confidence intervals are presented in Appendix E, Table 6. Maryland area-specific rates with 95% confidence intervals are presented in Appendix E, Table 14. Melanoma of the Skin There are three major types of skin cancer: basal cell carcinoma, squamous cell carcinoma, and melanoma. Incidence (New Cases) In 2014, a total of 1,452 cases of melanoma of the skin were reported in Maryland. Maryland had the 38 highest melanoma cancer mortality rate among the states and the District of Columbia for the period 2010-2014. In 2014, melanoma incidence rates were 86% higher among males than females in Maryland. Source: Maryland Cancer Registry 94 Mortality Trends by Gender Melanoma mortality rates in males decreased at a rate of 3. Source: Maryland Cancer Registry 95 Sun Exposure Protection the Healthy People 2020 target is increase 73. Department of Health and Human Services * the Healthy People 2020 estimate is based on adults who reported being very likely perform the following protective measures: limit sun exposure, use sunscreen, or wear protective clothing. Melanoma Age-Adjusted Incidence Rates* by Jurisdiction, Gender, and Race, Maryland, 2014 Gender Race Jurisdiction Total Males Females Whites Blacks Other Maryland 21. Melanoma Age-Adjusted Mortality Rates* by Jurisdiction, Gender, and Race, Maryland, 2014 Gender Race Jurisdiction Total Males Females Whites Blacks Other Maryland 2. Melanoma Age-Adjusted Incidence Rates* by Jurisdiction, Gender, and Race, Maryland, 2010-2014 Gender Race Jurisdiction Total Males Females Whites Blacks Other Maryland 21. Melanoma Age-Adjusted Mortality Rates* by Jurisdiction, Gender, and Race, Maryland, 2010-2014 Gender Race Jurisdiction Total Males Females Whites Blacks Other Maryland 2. Maryland area-specific rates with 95% confidence intervals are presented in Appendix E, Table 7. Maryland area-specific rates with 95% confidence intervals are presented in Appendix E, Table 15. Cervical Cancer Incidence (New Cases) A total of 215 cases of cervical cancer among women in Maryland were reported in 2014. Mortality (Deaths) In 2014, a total of 63 women died of cervical cancer in Maryland. Maryland had the 31 highest cervical cancer mortality rate among the states and the District of Columbia for the period 2010-2014. Source: Maryland Cancer Registry 108 Mortality Trends by Race From 2010 2014, mortality rates for black females decreased at a rate of 3. The proportion of cervical cancer cases reported as unstaged increased in 2014 9. Source: Maryland Cancer Registry 109 Cervical Cancer Screening One Healthy People 2020 target for cervical cancer is increase 93. Cervical Cancer Age-Adjusted Incidence Rates* by Jurisdiction and Race, Maryland, 2014 Race Jurisdiction Total Whites Blacks Other Maryland 6. Cervical Cancer Age-Adjusted Mortality Rates* by Jurisdiction and Race, Maryland, 2014 Race Jurisdiction Total Whites Blacks Other Maryland 1. Cervical Cancer Age-Adjusted Incidence Rates* by Jurisdiction and Race, Maryland, 2010-2014 Race Jurisdiction Total Whites Blacks Other Maryland 6. Cervical Cancer Age-Adjusted Mortality Rates* by Jurisdiction and Race, Maryland, 2010-2014 Race Jurisdiction Total Whites Blacks Other Maryland 2. Maryland area-specific rates with 95% confidence intervals are presented in Appendix E, Table 8. Maryland area-specific rates with 95% confidence intervals are presented in Appendix E, Table 16. The Maryland cancer reporting law and regulations mandate the collection of cancer information from Maryland-licensed hospitals, radiation therapy centers, diagnostic pathology laboratories, freestanding ambulatory care facilities, surgical centers, and physicians whose non-hospitalized cancer patients are not otherwise reported. Information on Maryland residents diagnosed and/or treated for cancer in these jurisdictions is included in this report. The number of deaths, crude death rates, and age-adjusted death rates can be obtained by place of residence (total U. Mortality data for the individual years 2005 2007 and 2012 2014 for Maryland and 2005 2008 for the U. Maryland mortality data for 2011 were obtained from the Maryland Vital Statistics Administration. The official annual reports from the Maryland Vital Statistics Administration can be obtained online at health. Comparisons can still be made between the different data sources for lung and bronchus cancer mortality due the small number of deaths due cancer of the trachea. Behavioral and Risk Factor Data the data on the prevalence of cancer screening and prevalence of various risk factors for cancer. This survey provided risk behavior and cancer screening information for this report. In 2013, a total of 53,785 students in 184 public high schools in Maryland completed the survey. In 2014, a total of 56,717 students in 183 public high schools in Maryland completed the survey. Because incidence data and mortality data come from different sources, separate suppression procedures were employed for release of non-confidential data. Age-adjusted incidence rates based on counts of 15 or fewer (non-zero) are presented with asterisks (**) because the rates are unstable and do not provide reliable information. In accordance with this policy, the following protocols are applied mortality data in this report: Death counts of 0-9 are suppressed, and denoted by <10. As a result, the totals shown in the count for number of cancer cases may not equal the sum of males and females because of cases in the other gender categories. As a result, the totals shown in the count for number of cancer cases may not equal the sum of the cancer cases across all 24 jurisdictions because of cases with unknown county. The individual year mortality data (2014) consist of deaths that occurred between January 1 and December 31 of that year. Age-adjustment, also called age-standardization, is a tool used control for different and changing age distributions of populations in the U. Age adjusted rates do not include cancer cases for which age has not been reported. Incidence and mortality rates in this report were calculated and age-adjusted using the 2000 U. Confidence Intervals and Statistical Significance Age-adjusted rates for specific geographic areas. It is important note however, that incidence and mortality rates, particularly those based on small numbers of events (cases or deaths) or small population sizes, can be highly variable from year year. In these instances, two unadjusted rates cannot be compared side-by-side determine whether they are statistically significantly different. A confidence interval is used describe the range of uncertainty around a point estimate. Confidence intervals are useful in defining a range within which the typical rate for a geographic area can be expected lie. Most confidence intervals are, by convention, calculated at the 95% level, which means that 95% of hypothetically observed confidence intervals generated will contain the true value of interest. The 129 smaller the number of events upon which a rate is based, the wider the confidence interval will be. Confidence intervals for incidence and mortality rates are included in this report facilitate comparisons between rates, such as the comparison of Maryland rates U. The following formula can be used approximate the 95% confidence interval for age-adjusted rates: Lower limit = R [1. Since these confidence intervals do not overlap, the two rates are considered be statistically significantly different. If the two confidence intervals overlap and if the rate for one area is included in the confidence interval of the other rate, then there is not a statistically significant difference between the rates. However, when there is overlap in the confidence intervals for two rates, and the rate for the comparison area is not included in the interval for the rate of interest, the two rates may or may not be statistically significantly different. National Comparison Data Maryland (statewide) and county incidence and mortality rates are compared U. Because mortality rates describe the cancer burden better than incidence rates, only Maryland rankings for mortality are presented for each targeted cancer. Maps included with this data display comparisons of Maryland incidence and mortality rates by geographical area U. Note that 10-25% includes 10% and 25%, but less than 10% and more than 25% do not include the endpoints of the range. The Other race category includes cases reported as American Indian or Alaskan Native, Asian or Pacific Islander, and any other race category, except those cases with unknown or missing race. However, only white, black, and other races are included in the Cancer Report, with the Other race category only including American Indian or Alaska Native and Asian or Pacific Islander cases. The derivation is an algorithm based on the person having a Hispanic surname (last or maiden name) and their country of birth, race, and sex. The category of Other races in this report includes the American Indian or Alaska Native race category and the Asian or Pacific Islander race category. We acknowledge the State of Maryland, the Maryland Cigarette Restitution Fund, and the National Program of Cancer Registries of the Centers for Disease Control and Prevention for the funds that support the collection and availability of the cancer registry data. The findings and conclusions of this report are those of the authors and do not necessarily represent the views of the Maryland Department of Health. This policy prohibits discrimination on the basis of race, color, sex, or national origin and applies the provisions of employment and granting of advantages, privileges and accommodations. Breast cancer Medical Director, Texas Life Insur detection, treatment, and prevention are prominent issues in public ance Company. Background information on develop ments in these arenas is provided so that medical directors can con Key words: Breast cancer, ductal tinue update their approach the assessment of breast cancer carcinoma in situ, lobular carcino risk. Breast cancers are divided into means that 70% 75% of women with in 2 major types, in situ carcinomas and invasive vasive breast cancer will die of something oth (or in? Chances of a Woman Developing Breast Cancer by Age curve at younger ages, the more important issue is the increasing prevalence of breast By Age Normal Risk Genetic Risk* cancer with advancing age, and the take 45 1 in 93 (1%) 42% home message for physicians and underwrit 55 1 in 33 (3%) 72% ers alike is that any breast mass in a post 65 1 in 17 (6%) 80% menopausal woman should be considered 75 1 in 11 (9%) 84% 8 cancer until proven otherwise. The potential for metastases and ulti breasts, or if it occurred in conjunction with ovarian cancer. Thus, environmental and/or life strual cycles and thus greater hormone ex style factors appear be important deter posure. In women, incidence trogen plus progestin with placebo on chron rates of breast cancer rise sharply with age ic disease risk, con? The percentages and distribution of in In contrast, among women taking estrogen, vasive ductal, invasive lobular, mixed ductal, those who gained weight did not have an in and lobular as well as tubular carcinomas creased risk of breast cancer. The differing ef were similar in the estrogen plus progestin fects of obesity and weight gain in premen group vs the placebo group. Therefore, pre late metabolism that protects against tumor vious breast cancer is an accepted risk factor growth. Acute enlargement of cysts ation after age 45 does not confer increased may cause pain, and because breast ducts are risk. The most vulnerable ages appear be usually patent, nipple discharge is common the prepubertal years of 10 14. These wom with the discharge varying in color from pale en should have yearly mammograms and green brown. The number, size and shape this is an issue of great concern for pa of epithelial cells lining the basement mem tients, physicians and insurance companies brane of ducts are increased, but the histolo alike, as there are conditions that confer no gy does not ful?
In addition antibiotic cream for dogs buy discount minocin 50 mg on line, the adverse reactions in Study 19 that occurred in <20% of patients receiving Lynparza were dyspepsia antimicrobial herbs and spices buy minocin master card, stomatitis antibiotics for dogs abscess discount minocin 50mg on-line, dysgeusia antibiotic resistance peer reviewed journal order minocin cheap online, dizziness antimicrobial yoga mats buy minocin with a visa, increase in creatinine bacteria yeast and mold discount minocin 50 mg visa, neutropenia, thrombocytopenia, leukopenia, lymphopenia, dyspnea, pyrexia and edema. Adverse reactions led dose interruption in 40% of patients, dose reduction in 4% of patients, and discontinuation in 7% of patients. The following adverse reactions and laboratory abnormalities have been identified in? Dose interruptions due an adverse reaction of any grade occurred in 35% of patients receiving Lynparza and 28% of those receiving chemotherapy; dose reductions due an adverse reaction occurred in 25% of Lynparza patients and 31% of chemotherapy patients. Discontinuation occurred in 5% of Lynparza patients and 8% in chemotherapy patients. Represents grouped terms consisting of anemia (anemia erythropenia, hematocrit decreased, hemoglobin decreased and red blood cell count decreased). Represents grouped terms consisting of leukopenia (leukopenia and white blood cell count decreased). Represents grouped terms consisting of neutropenia (febrile neutropenia, granulocyte count decreased, granulocytopenia, neutropenia, neutropenic infection, neutropenic sepsis, neutrophil count decreased). Represents grouped terms consisting of bronchitis, influenza, lower respiratory tract infection, nasopharyngitis, pharyngitis, respiratory tract infection, rhinitis, sinusitis, upper respiratory tract infection, upper respiratory tract infection bacterial. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible reliably estimate their frequency or establish a causal relationship drug exposure. There are no available data on Lynparza use in pregnant women inform the drug-associated risk. In an animal reproduction study, the administration of olaparib pregnant rats during the period of organogenesis caused teratogenicity and embryo-fetal toxicity at exposures below those in patients receiving the recommended human dose of 300 mg twice daily [see Data]. Apprise pregnant women of the potential hazard the fetus and the potential risk for loss of the pregnancy. The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. Additional abnormalities or variants included incomplete or absent ossification (vertebrae/sternebrae, ribs, limbs) and other findings in the vertebrae/sternebrae, pelvic girdle, lung, thymus, liver, ureter and umbilical artery. Some findings noted above in the eyes, ribs and ureter were observed at a dose of 0. Because of the potential for serious adverse reactions in the breastfed infants from Lynparza, advise a lactating woman not breastfeed during treatment with Lynparza and for one month after receiving the last dose. Contraception Females Lynparza can cause fetal harm when administered a pregnant woman [see Use in Specific Populations (8. Advise females of reproductive potential use effective contraception during treatment with Lynparza and for at least 6 months following the last dose. Males Based on findings in genetic toxicity and animal reproduction studies, advise male patients with female partners of reproductive potential or who are pregnant use effective contraception during treatment and for 3 months following the last dose of Lynparza. Advise male patients not donate sperm during therapy and for 3 months following the last dose of Lynparza [see Use in Specific Populations (8. No overall differences in the safety or effectiveness of Lynparza were observed between younger and older patients. There are no data in patients with moderate or severe hepatic impairment [see Clinical Pharmacology (12. For patients with moderate renal impairment, reduce the dose of Lynparza 200 mg twice daily [see Dosage and Administration (2. In the event of an overdose, physicians should follow general supportive measures and should treat the patient symptomatically. Olaparib is a crystalline solid, is non-chiral and shows pH-independent low solubility across the physiological pH range. Inactive ingredients in the tablet core are copovidone, mannitol, colloidal silicon dioxide and sodium stearyl fumarate. The tablet coating consists of hypromellose, polyethylene glycol 400, titanium dioxide, ferric oxide yellow and ferrosoferric oxide (150 mg tablet only). Olaparib has been shown inhibit growth of select tumor cell lines in vitro and decrease tumor growth in mouse xenograft models of human cancer, both as monotherapy or following platinum based chemotherapy. The oral bioavailability of the tablet formulation is higher than the capsule formulation. Absorption Following oral administration of olaparib, absorption is rapid with median peak plasma concentrations typically achieved 1. Co-administration of a high fat meal with olaparib slowed the rate (tmax delayed by 2. Distribution Olaparib had a mean ( standard deviation) apparent volume of distribution of 158 136 L after a single 300 mg dose of olaparib. Following oral dosing of 14C-olaparib female patients, unchanged olaparib accounted for the majority of the circulating radioactivity in plasma (70%). It was extensively metabolized with unchanged drug accounting for 15% and 6% of radioactivity in urine and feces, respectively. Following a single dose of 14C-olaparib, 86% of the dosed radioactivity was recovered within a 7-day collection period, 44% via the urine and 42% via the feces. Mild hepatic impairment had no effect on the protein binding of olaparib and therefore total plasma exposure was representative of free drug. This clastogenicity is consistent with genomic instability resulting from the primary pharmacology of olaparib and indicates potential for genotoxicity in humans. Randomization was stratified by response last platinum chemotherapy (complete versus partial) and time disease progression in the penultimate platinum-based chemotherapy prior enrollment (6-12 months versus > 12 months). All patients had received at least two prior platinum-containing regimens and were in response (complete or partial) their most recent platinum-based regimen. Prior bevacizumab therapy was reported for 17% of those treated with Lynparza and 20% of those receiving placebo. Approximately 44% of patients on the Lynparza arm and 37% on placebo had received three or more lines of platinum-based treatment. Hazard ratio from the stratified proportional hazards model, stratified by response last platinum chemotherapy (complete versus partial) and time disease progression in the penultimate platinum-based chemotherapy prior enrollment. The median age of patients treated with Lynparza (n=136) was 58 years (range: 21 89) and 59 years (range 33 84) among patients treated with placebo (n=129). Prior bevacizumab therapy was reported for 13% of patients receiving Lynparza and 16% of patients receiving placebo. Table 10 Efficacy Results Study 19 (Investigator Assessment) Lynparza capsules Placebo (n=136) (n=129) Progression-Free Survival Number of events (%) 60 (44%) 94 (73%) Median, months 8. Hazard ratio is derived from a stratified proportional hazards model, stratified by response last platinum chemotherapy, time disease progression in the penultimate platinum-based chemotherapy and Jewish and non-Jewish descent. All patients received Lynparza capsules at a dose of 400 mg twice daily as monotherapy until disease progression or intolerable toxicity. Randomization was stratified by prior use of chemotherapy for metastatic disease (yes vs no), hormone receptor status (hormone receptor positive vs triple negative), and previous use of platinum-based chemotherapy (yes vs no). Patients were required have received treatment with an anthracycline (unless contraindicated) and a taxane, in the neoadjuvant, adjuvant or metastatic setting. Patients with hormone receptor-positive disease must have progressed on at least 1 endocrine therapy (adjuvant or metastatic), or have disease that the treating healthcare provider believed be inappropriate for endocrine therapy. Patients with prior platinum therapy were required have no evidence of disease progress during platinum treatment. Approximately 50% of patients had triple-negative tumors and 50% had estrogen receptor and/or progesterone receptor positive tumors and the proportions were balanced across treatment arms. Patients in each treatment arm had received a median of 1 prior chemotherapy regimen for metastatic disease; approximately 30% had not received a prior chemotherapy regimen for metastatic breast cancer. Twenty-one percent of patients in the Lynparza arm and 14% in the chemotherapy arm had received platinum therapy for metastatic disease. Seven percent of patients in each treatment arm had received platinum therapy for localized disease. Consistent results were observed across patient subgroups defined by study stratification factors. Instruct patients that if they miss a dose of Lynparza, they should take their next normal dose at the usual time. Inform patients avoid grapefruit, grapefruit juice, Seville oranges, and Seville orange juice while taking Lynparza [see Drug Interactions (7. Inform female patients of the risk a fetus and potential loss of the pregnancy [see Use in Specific Populations (8. Advise females of reproductive potential use effective contraception during treatment with Lynparza and for 6 months after the last dose. Advise male patients with female partners of reproductive potential or who are pregnant use effective contraception during treatment and for 3 months after receiving the last dose of Lynparza. Advise male patients not donate sperm during therapy and for 3 months following the last dose of Lynparza [see Warnings and Precautions (5. Your healthcare provider may stop treatment with Lynparza until your blood cell counts improve. Tell your healthcare provider if you have any new or worsening symptoms of lung problems, including shortness of breath, fever, cough, or wheezing. Your healthcare provider may temporarily or completely stop treatment if you develop pneumonitis. You should have received chemotherapy medicines, either before or after your cancer has spread. Your healthcare provider will perform a test make sure that Lynparza is right for you. Talk your healthcare provider about birth control methods that may be right for you. Do not breastfeed during treatment with Lynparza and for 1 month after receiving the last dose of Lynparza. Talk your healthcare provider about the best way feed your baby during this time. Tell your healthcare provider about all the medicines you take, including prescription and over-the counter medicines, vitamins, and herbal supplements. Taking Lynparza and certain other medicines may affect how Lynparza works and may cause side effects. If your healthcare provider prescribes Lynparza tablets for you, do not take Lynparza capsules. If you have any questions about Lynparza, please talk your healthcare provider or pharmacist. General information about the safe and effective use of Lynparza Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not give Lynparza other people, even if they have the same symptoms you have. You can ask your healthcare provider or pharmacist for information about Lynparza that is written for health professionals. Active ingredient: olaparib Inactive ingredients: Tablet contains: copovidone, mannitol, colloidal silicon dioxide and sodium stearyl fumarate Tablet coating contains: hypromellose, polyethylene glycol 400, titanium dioxide, ferric oxide yellow and ferrosoferric oxide (150 mg tablet only) Lynparza is a registered trademark of the AstraZeneca group of companies. It has been associated with an increased risk exercise and hyperlipidaemia on the immune microenviron of developing breast cancer, as well as with a poorer progno ment of tumours is analysed. It has been shown that adipocytes in the investigated circulating factors as exercise-modulated, pro immediate vicinity of the tumour (cancer associated gnostic biomarkers is also discussed. We propose that exerci adipocytes) interact with breast cancer cells, causing them se may alleviate some of the pro-tumorigenic effects of hyper become more invasive and providing them with metabolites lipidaemia through the reduction of blood lipid levels and (145). In addition, obese adipose tissue is characterised by modulation of cytokine release induce beneficial changes in chronic, low-grade inflammation. It is the most com mon cancer diagnosed in women (193) and the fifth largest Hyperlipidaemia is commonly comorbid with obesity, but its contributor cancer deaths worldwide (23). As such, under implications as an independent risk or prognostic factor in standing the underlying mechanisms of disease progression is breast cancer are much less clear. In addition, the purpose of this review is explore the association breast tumours from hyperlipidaemic mice are more prolifera between exercise and (breast) cancer progression, and high tive (100, 153, 163), have reduced apoptosis (153) and show light potential mechanisms underlying the exercise-prognosis increased microvessel density (100, 112, 153). Types of exercise include resistance training, aer However, epidemiological studies have produced contradicto obic exercise and training that includes a mindfulness compo ry results regarding the effect of hyperlipidaemia, particularly nent such as Tai chi or yoga. The role of obesity and associat hypercholesterolaemia, on breast cancer risk and progression, ed hyperlipidaemia (abnormal elevation of serum lipid levels) with some studies showing that hyperlipidaemia increases risk and/or progression (10, 43, 97, 101, 157, 164), and others showing that it reduces or does not change risk and/or rate of progression (42, 58, 65, 177, 183). In connection with this, the role of statins and other lipid lowering drugs on breast cancer risk and progression is unclear (26, 42, 97, 104, 138, 159, 186). However, two recent meta-analyses of observational studies found that statin use was associated with reduced breast cancer recurrence and/or mortality (121, 204). These * Corresponding author: discrepancies may be due the inherent limitations of epi Associate Professor G. Dachs, demiological studies, as well as differences in methodology, University of Otago Christchurch, 2 Riccarton Ave, Christchurch 8011, New Zealand; gabi. The authors of that study suggest that cholesterol-induced tumour progres sion could be mediated by androgen signalling or mono cyte/macrophage recruitment (153); however both hypotheses are yet be validated. Thus, further studies are neces sary elucidate the mechanism(s) behind the more rapid tumour growth and increased metastasis occurring in a hyper lipidaemic host. Hyperlipidaemia and Immunity the impact of hyperlipidaemia on host immunity is complex, with studies indicating both an impairment of immunity resulting in increased susceptibility infection (102, 114), and a reduction in tolerance through reduced functionality of regulatory T cells (Treg cells) (9). Oxysterols, formed during Figure 1: Potential Mechanisms of Cholesterol in Breast Cancer Pro cholesterol metabolism, are well known play a role in regu gression. In addition, it may increase macrophage recruitment, activate sterols and in vitro experiments with synthetic oxysterols. In this regard, exercise may inhibit cancer progression ther survival benefit was seen with increasing exercise levels and development in hyperlipidaemic individuals through the (106). With respect exercise type, resistance and aerobic reduction of chronic inflammation. It seems that post-diagnosis exercise has a larger effect and reduce the risk of cardiovascular disease (140). In addi on survival than pre-diagnosis exercise, although the wide tion, it can lower serum lipid levels (120).
Buy discount minocin online. Antimicrobial Resistance (AMR) explained with magic ENGLISH SUBTITLES - ABMU Pacesetter Project.