Patricia B. Crawford DrPH, RD
- Adjunct Professor

https://publichealth.berkeley.edu/people/patricia-crawford/
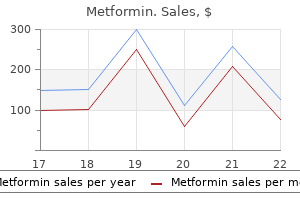
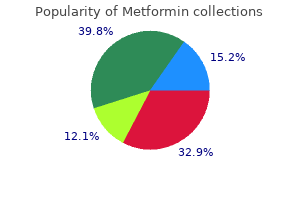
Contusions and hematomas of the chest Perineum diabetes symptoms on feet generic 500 mg metformin fast delivery, Rectum diabetes insipidus in dogs diet purchase metformin 850mg without prescription, and Vagina wall will alert the clinician to the possibility of occult injury diabetic rice purchase metformin online pills. The perineum should be examined for contusions diabetes in dogs cost of insulin cheap 500mg metformin with amex, Signifcant chest injury can manifest with pain blood sugar levels order 850mg metformin mastercard, hematomas blood sugar elevated after surgery cheap 500mg metformin, lacerations, and urethral bleeding. Auscultation is conducted high the presence of blood within the bowel lumen, integrity on the anterior chest wall for pneumothorax and of the rectal wall, and quality of sphincter tone. Although Vaginal examination should be performed in patients auscultatory fndings can be difcult to evaluate in who are at risk of vaginal injury. Palpation of the bones and examination Rib fractures may be present, but they may not be visible on an x-ray. Identifying the specifc injury is less in patients with fractures, as important than determining whether operative clots can become dislodged intervention is required. Pain on palpation of the pelvic ring is an movement of an extremity or important finding in alert patients. In addition, response to stimulus of an assessment of peripheral pulses can identify area, may be the only clues vascular injuries. Impaired sensation and/or loss of voluntary muscle contraction strength can be caused by nerve injury or ischemia, including that due Specialized diagnostic tests may be performed during to compartment syndrome. Often these Early consultation with a neurosurgeon is required procedures require transportation of the patient to for patients with head injury. Monitor patients other areas of the hospital, where equipment and frequently for deterioration in level of consciousness personnel to manage life-threatening contingencies and changes in the neurologic examination, as these may not be immediately available. Therefore, fndings can refect worsening of an intracranial these specialized tests should not be performed injury. If a patient with a head injury deteriorates until the patient has been carefully examined neurologically, reassess oxygenation, the adequacy and his or her hemodynamic status has been of ventilation and perfusion of the brain. Other injuries can mask the physical fndings of spinal injuries, and they can remain undetected unless the clinician obtains the appropriate x-rays. Any evidence of loss of sensation, paralysis, or weakness suggests major injury to the spinal column or peripheral nervous system. Neurologic defcits should be documented when identifed, even when transfer to another facility or doctor for specialty care is necessary. Protection of the spinal cord is required at all times until a spine injury is excluded. Meticulous record keeping is crucial during patient Continuous monitoring of vital signs, oxygen assessment and management, including documenting saturation, and urinary output is essential. In pediatric patients who are older than essential for subsequent practitioners to evaluate the 1 year, an output of 1 mL/kg/h is typically adequate. See Sample Trauma doses to achieve the desired level of patient comfort Flow Sheet and Chapter 13: Transfer to Defnitive Care. The closest teAmwoRk appropriate local facility is chosen, based on its overall capabilities to care for the injured patient. The topic of transfer is described in more detail in Chapter 13: whose size and composition varies from institution to Transfer to Defnitive Care. The team leader supervises the by verbalizing each action and each fnding out loud preparation for the arrival of the patient to ensure a without more than one member speaking at the same smooth transition from the prehospital to hospital time. He or she assigns roles and tasks to terms, but instead are directed to an individual, by the team members, ensuring that each participant name. That individual then repeats the request/order has the necessary training to function in the and later confrms its completion and, if applicable, assigned role. He or she also orders additional examinations assessment and management and, when appropriate, suggests/directs transfer of the patient. To perform effectively, each team has one member who again considering the need for transfer. The primary survey should be repeated fre more is associated with increased mortality in quently, and any abnormalities will prompt a elderly and nonelderly trauma patients. Early identifcation of patients requiring transfer Video registration of trauma team performance to a higher level of care improves outcomes. Teamwork and patient safety in dynamic domains of healthcare: a review of the literature. Validation of patients with severe and multiple traumatic of prehospital trauma triage criteria for motor injuries. Preventable or potentially preventable Surgeons and the Advanced Trauma Life Support mortality at a mature trauma center. Pressure ulcers from spinal immobilization in document for the prehospital use of Tranexamic trauma patients: a systematic review. Guidelines for feld triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. Evaluation of trauma team performance using an advanced human patient simulator for resuscitation training. Recognize ventilatory compromise and signs of oxygenation before, during, and after establishing a inadequate ventilation. Therefore, to the brain and other vital structures is the initial assessment and frequent reassessment of airway T quickest killer of injured patients. In fact, securing a provides momentary reassurance that the airway is compromised airway, delivering oxygen, and sup patent and not compromised. Therefore, the most porting ventilation take priority over management of important early assessment measure is to talk to the all other conditions. Maintaining oxygenation There are many strategies and equipment choices and preventing hypercarbia are critical in managing for managing the airway in trauma patients. It is of trauma patients, especially those who have sustained fundamental importance to take into account the head injuries. For this reason, that are well known and regularly used in the specifc consider preemptive intubation in burn patients. AiRwAy the frst steps toward identifying and managing potentially life-threatening airway compromise are to recognize objective signs of airway obstruction and identify any trauma or burn involving the face, neck, and larynx. Although it is often related to pain or anxiety, injuries are at risk for insidious respiratory compromise, so consider or both, tachypnea can be a subtle but early sign of preemptive intubation. In this case, immediately suction and rotate the Endotracheal intubation may be necessary to maintain entire patient to the lateral position while restricting airway patency. Both blunt and penetrating neck injury can cause Maxillofacial Trauma disruption of the larynx or trachea, resulting in airway obstruction and/or severe bleeding into the Trauma to the face demands aggressive but careful airway tracheobronchial tree. Trauma to the midface can produce fractures into the soft tissues can cause partial airway obstruction. Facial fractures can be associated may be able to maintain airway patency and ventilation. Fractures of the mandible, airway injury, insert an endotracheal tube cautiously especially bilateral body fractures, can cause loss of and preferably under direct visualization. Loss of airway normal airway structural support, and airway obstruction patency can be precipitous, and an early surgical airway can result if the patient is in a supine position. Furthermore, providing general anesthesia, sedation, Laryngeal Trauma Although laryngeal fractures rarely occur, they can present with acute airway obstruction. Palpable fracture Complete obstruction of the airway or severe respiratory distress from partial obstruction warrants an attempt at intubation. Flexible endoscopic intuba tion may be helpful in this situation, but only if it can be performed promptly. Surgical cricothyroidotomy, belligerent patients may in fact be hypoxic; do although not preferred in this situation, can be a not assume intoxication. Penetrating trauma to the larynx or trachea can be overt and require immediate management. Complete veNtilAtioN tracheal transection or occlusion of the airway with blood or soft tissue can cause acute airway compromise requiring immediate correction. These injuries are Ensuring a patent airway is an important step in often associated with trauma to the esophagus, carotid providing oxygen to patients, but it is only the frst artery, or jugular vein, as well as soft tissue destruction step. Therefore, clinicians must Noisy breathing indicates partial airway obstruction look for any objective signs of inadequate ventilation. Patients with objective signs of airway difculty or Pediatric patients may sufer signifcant thoracic injury limited physiological reserve must be managed with without rib fractures. This applies, among others, to obese Intracranial injury can cause abnormal breathing patients, pediatric patients, older adults, and patients patterns and compromise adequacy of ventilation. Cervical spinal cord injury can result in respiratory the following steps can assist clinicians in identify muscle paresis or paralysis. The more proximal ing objective signs of airway obstruction: the injury, the more likely there will be respiratory impairment. Observe the patient to determine whether maintenance of the diaphragmatic function but loss he or she is agitated (suggesting hypoxia) or of the intercostal and abdominal muscle contribution obtunded (suggesting hypercarbia). Typically these patients display a seesaw indicates hypoxemia from inadequate pattern of breathing in which the abdomen is pushed oxygenation and is identifed by inspecting out with inspiration, while the lower ribcage is pulled the nail beds and circumoral skin. Pulse oximetry used early in the airway assessment can detect inadequate oxygenation objeCtiVe signs oF inadeqUate before cyanosis develops. Snoring, gurgling, the following steps can assist clinicians in identifying and crowing sounds (stridor) can be associated objective signs of inadequate ventilation: with partial occlusion of the pharynx or larynx. Use capnography in spontaneously breathing and cage, pneumothorax, or a fail chest. Labored intubated patients to assess whether ventilation breathing may indicate an imminent threat to is adequate. Decreased or absent breath sounds over one or both hemithoraces should alert the examiner to the presence of thoracic injury. Note, however, that this device measures to improve oxygenation and reduce the risk does not measure the adequacy of ventilation. These measures Additionally, low oxygen saturation can be an include airway maintenance techniques, defnitive indication of hypoperfusion or shock. While one person restricts movement of the cervical spine, (A), the second person expands the helmet laterally. The second person then removes the helmet (B), while ensuring that the helmet clears the nose and occiput. This is a two-person procedure: One person When such difficulties are encountered, skilled restricts cervical spinal motion from below while the clinicians should assist. Using a cast cutter to remove the helmet several of its components are particularly relevant while stabilizing the head and neck can minimize in trauma. Rely on clinical judgment and experience way to predict the difculty of the maneuver. Factors in determining whether to proceed immediately with that indicate potential difficulties with airway drug-assisted intubation.
Listen with the diaphragm at the left 2nd interspace near the sternum (pulmonic area) diabetes symptoms glucose in urine purchase metformin online now. Listen with the diaphragm at the left 3rd diabetes mellitus urine specific gravity cheap metformin 500mg fast delivery, 4th blood sugar refers to what molecule circulating in blood generic 500mg metformin with visa, and 5th interspaces near the sternum (tricuspid area) type 1 diabetes quizlet purchase discount metformin line. Record S1 diabetes diet kenya order on line metformin, S2 diabetes mellitus type 2 cpg malaysia generic metformin 850mg on line, (S3), (S4), as well as the grade and configuration of any murmurs ("two over six" or "2/6", "pansystolic" or "crescendo"). Grade i-ii functional systolic murmurs are common in young children and resolve with age 2. Heard only if room silent and then still hard to hear ii Clearly audible, but faint iii Moderately loud, easy to hear iv Loud, associated with thrill on chest wall v Very loud, can hear with edge of stethoscope off chest vi Loudest, can hear with entire stethoscope off chest wall Edema, Cyanosis, and Clubbing 1. Examination of the Abdomen Equipment Needed Stethoscope General Considerations 1. The examination room must be quiet to perform adequate auscultation and percussion. Page 20 of 35 Adapted from the Kentucky Public Health Practice Reference, 2008 and Jarvis, C, (2011). Percuss downward from the chest in the right midclavicular line until you detect the top edge of liver dullness. Percuss upward from the abdomen in the same line until you detect the bottom edge of liver dullness. Alternate Method this method is useful when the patient is obese or when the examiner is small compared to the patient. A well defined, pulsatile mass, greater than 3 cm across, suggests an aortic aneurysm. Page 21 of 35 Adapted from the Kentucky Public Health Practice Reference, 2008 and Jarvis, C, (2011). Measure the distance around the abdomen at a specific point, usually at the level of the belly button (navel). Use the heel of your closed fist to strike the patient firmly over the costovertebral angles. If the dullness has shifted to areas of prior tympany, the patient may have excess peritoneal fluid. Not used as much lately as there is a question on how well it predicts appendicitis F. Often need to assess standing up ***************************************************************************************** Page 22 of 35 Adapted from the Kentucky Public Health Practice Reference, 2008 and Jarvis, C, (2011). Some portions of the examination may not be appropriate depending on the clinical situation (performing range of motion on a fractured leg for example). Think of the underlying anatomy as you obtain the history and examine the patient. When taking a history for an acute problem always inquire about the mechanism of injury, loss of function, onset of swelling (< 24 hours), and initial treatment. When taking a history for a chronic problem always inquire about past injuries, past treatments, effect on function, and current symptoms. The cardinal signs of musculoskeletal disease are pain, redness (erythema), swelling, increased warmth, deformity, and loss of function. With Musculoskeletal system, Always begin with inspection, palpation and range of motion, regardless of the region you are examining (except abdomen). A complete evaluation will include a focused neurologic exam of the affected area. Always consider referred pain, from the neck or chest to the shoulder, from the back or pelvis to the hip, and from the hip to the knee. Diagnostic hints based on location of pain: Back Side Front Shoulder Pain Muscle Spasm Bursitis or Rotator Cuff Glenohumeral Joint Hip Pain Sciatica Bursitis Hip Joint Inspection 1. Start by asking the patient to move through an active range of motion (joints moved by patient). Proceed to passive range of motion (joints moved by examiner) if active range of motion is abnormal. Page 23 of 35 Adapted from the Kentucky Public Health Practice Reference, 2008 and Jarvis, C, (2011). If increased range of motion is detected, perform special tests for instability as appropriate. Shoulder flexion/extension; internal/external rotation; abduction/adduction (2/3 glenohumeral joint, 1/3 scapulo-thoracic) 7. Identify the "anatomic snuffbox" between the extensor pollicis longus and brevis (extending the thumb makes these structures more prominent). Page 24 of 35 Adapted from the Kentucky Public Health Practice Reference, 2008 and Jarvis, C, (2011). If the rotator cuff (especially the supraspinatus) is torn, the patient will be unable to lower the arm slowly and smoothly. Significant shoulder pain as the arm is raised suggests an impingement of the rotator cuff against the acromion. Hold the metacarpophalangeal and proximal interphalangeal joints of the finger being tested in extension. Ask the patient to press the backs of the hands together with the wrists fully flexed (backward praying). Have the patient hold this position for 60 seconds and then comment on how the hands feel. Pain, tingling, or other abnormal sensations in the thumb, index, or middle fingers strongly suggest carpal tunnel syndrome. If the knee joint "opens up" medially, the medial collateral ligament may be torn. If the knee joint "opens up" laterally, the lateral collateral ligament may be torn. Page 25 of 35 Adapted from the Kentucky Public Health Practice Reference, 2008 and Jarvis, C, (2011). Ask the patient to lie supine on the exam table with knees flexed to 90 degrees and feet flat on the table. If the tibia moves out from under the femur, the anterior cruciate ligament may be torn. If the tibia moves back under the femur, the posterior cruciate ligament may be torn. If the patella visibly rebounds, a large knee effusion (excess fluid in the knee) is present. Tap gently over the collected fluid and observe the effect on the lateral side, or ballot the patella as outlined above. Abnormal = presence of pain occurs with other conditions but a deep vein thrombosis should be ruled out. Pain in an L5 or S1 distribution suggests nerve root compression or tension (radicular pain). Increased pain on the opposite side indicates that a nerve root problem is almost certain. This test is used to distinguish hip or sacroiliac joint pathology from spine problems. Place the foot of the effected side on the opposite knee (this flexes, abducts, and externally rotates the hip). Press down gently but firmly on the flexed knee and the opposite anterior superior iliac crest. Page 26 of 35 Adapted from the Kentucky Public Health Practice Reference, 2008 and Jarvis, C, (2011). Organize your thinking into seven categories: a) Mental Status b) Cranial Nerves c) Motor d) Coordination and Gait e) Reflexes f) Sensory g) Special Tests Mental Status: 1. Assess level of consciousness; facial expression and body language; speech; cognition and functioning 2. Test Visual Acuity: Use Snellen eye chart or a Rosenbaum pocket card at a 14 inch "reading" distance). Substitute a blunt object occasionally and ask the patient to report "sharp" or "dull. If you find and abnormality then: Test the three divisions for temperature sensation with a tuning fork heated or cooled by water. Mixed: (A) Motor: muscles used for facial expressions, close eye and mouth; (B) Sensory (sense of taste in the front 2/3 of tongue; (C) Parasympathetic: saliva and tear secretion 2. Observe for Any Facial Droop or Asymmetry a) Ask Patient to do the following, note any lag, weakness, or asymmetry: Raise eyebrows b) Close both eyes to resistance c) Smile d) Frown e) Show teeth f) Puff out cheeks 4. Initial test: a) Face the patient and hold out your arms with your fingers near each ear. Page 28 of 35 Adapted from the Kentucky Public Health Practice Reference, 2008 and Jarvis, C, (2011). Abnormal indicates conductive hearing loss in that ear or sensory hearing loss in opposite ear. Mixed: motor: (A) Motor: pharynx (phonation and swallowing); (B) Sensory: taste on posterior 1/3 of tongue; gag reflex; (C) parasympathetic: parotid gland, carotid reflex. On an unconscious or uncooperative patient, stimulate the back of the throat on each side. Move tongue from side to side Page 29 of 35 Adapted from the Kentucky Public Health Practice Reference, 2008 and Jarvis, C, (2011). Grade strength on a scale from 0 to 5 "out of five": Grading Motor Strength Grade Description 0/5 No muscle movement 1/5 Visible muscle movement, but no movement at the joint 2/5 Movement at the joint, but not against gravity 3/5 Movement against gravity, but not against added resist 4/5 Movement against resistance, but less than normal 5/5 Normal strength Test the following: 1. Ask the patient to stand for 20-30 seconds with both arms straight forward, palms up, and eyes closed. The patient will not be able to maintain extension and supination (and "drift into pronation) with upper motor neuron disease. Page 30 of 35 Adapted from the Kentucky Public Health Practice Reference, 2008 and Jarvis, C, (2011). Ask the patient to strike one hand on the thigh, raise the hand, turn it over, and then strike it back down as fast as possible. Ask the patient to tap the distal thumb with the tip of the index finger as fast as possible. Ask the patient to touch your index finger and their nose alternately several times. Hold your finger still so that the patient can touch it with one arm and finger outstretched. Ask the patient to move their arm and return to your finger with their eyes closed. Ask the patient to place one heel on the opposite knee and run it down the shin to the big toe. Ask the patient to stand with the feet together and eyes closed for 5-10 seconds without support. The test is said to be positive if the patient becomes unstable (indicating a vestibular or proprioceptive problem). Reflexes can be reinforced by having the patient perform isometric contraction of other muscles (clenched teeth). Exaggerated hyperactive reflexes in a pregnant woman may be related to pre-eclampsia. Reflexes should be graded on a 0 to 4 "plus" scale: Tendon Reflex Grading Scale Grade Description 0 Absent 1+ or + Hypoactive 2+ or ++ "Normal" 3+ or +++ Hyperactive without clonus May indicate disease but also may be normal 4+ or ++++ Hyperactive with clonus Indicative of disease (see definition below) Page 31 of 35 Adapted from the Kentucky Public Health Practice Reference, 2008 and Jarvis, C, (2011). Abdominal (T8, T9, T10, T11, T12) Use a blunt object such as a key or tongue blade. Stroke the abdomen lightly on each side in an inward and downward direction above (T8, T9, T10) and below the umbilicus (T10, T11, T12). Note the contraction of the abdominal muscles and deviation of the umbilicus towards the stimulus. If the reflexes seem hyperactive, test for ankle clonus: a) Support the knee in a partly flexed position. Stroke the lateral aspect of the sole of each foot with the end of a reflex hammer or key. Extension of the big toe with fanning of the other toes is abnormal in other than a young child. Page 32 of 35 Adapted from the Kentucky Public Health Practice Reference, 2008 and Jarvis, C, (2011). Test with a non-vibrating tuning fork first to ensure that the patient is responding to the correct stimulus. If vibration sense is impaired proceed proximally: a) Wrists b) Elbows c) Medial malleoli d) Patellas e) Anterior superior iliac spine f) Spinous processes g) Clavicle Position Sense 1. If indicated move proximally to the metacarpophalangeal joints, wrists, and elbows. If vibration, position sense, and subjective light touch are normal in the fingers and toes you may assume the rest of this exam will be normal. Test the following areas: a) Shoulders (C4) b) Inner and outer aspects of the forearms (C6 and T1) c) Thumbs and little fingers (C6 and C8) d) Front of both thighs (L2) e) Medial and lateral aspect of both calves (L4 and L5) f) Little toes (S1) Page 33 of 35 Adapted from the Kentucky Public Health Practice Reference, 2008 and Jarvis, C, (2011). Use a tuning fork heated or cooled by water and ask the patient to identify "hot" or "cold.
Purchase metformin amex. Weight loss journey for Type 1 Diabetes...
Although the available data associate a medical benefit and economic benefit [9] to neonatal circumcision diabetes diet type 2 buy generic metformin 850mg, previously conducted clinical studies have been criticized for potential selection and sampling bias [44] diabetes type 2 death generic metformin 500 mg without a prescription. The flora of the colon and urogenital region is a result of native host immunity diabetes diet recipes for desserts order metformin 850 mg fast delivery, existing microbial ecology diabetes type 1 research news order line metformin, and the presence of microbe-altering drugs and foods diabetic diet meal ideas generic metformin 850mg without prescription. A recent investigation by Schlager and colleagues [12] sup ported the theory that a subset of the colonic microflora expressing particular virulence factors is most likely to infect the urinary tract diabetes signs skin cheap metformin 850mg with amex. Infections associated with urinary tract malformation generally appear in children younger than 5 years of age. Surgical intervention may be required to correct the anatomic abnormality (see Box 1). These urinary tract malformations increase the likelihood that infections of the lower urinary tract (ie, bladder and urethra) will ascend to the upper tracts with possible pyelonephritis and potential renal deterioration [48]. Importantly, children with known urinary malformation may be on chronic antimicrobial prophylaxis. Inability to empty the bladder, as in the case of neuro genic bladders, frequently results in urinary retention, urinary stasis, and subopti mal clearance of bacteria from the urinary tract. Clean intermittent catheterization is helpful for emptying the neurogenic bladder, but catheterization itself may introduce bacteria to this normally sterile space. Uropathogenic strains of E coli also are more likely to be shared during sexual intercourse than commensal E coli [57]. The physical examination is pediatric urinary tract infections 387 also frequently of limited value because costovertebral angle and suprapubic tenderness are not reliable signs in the pediatric population. In older children younger than 2 years, the most common symptoms include fever, vomiting, anorexia, and failure to thrive [60]. Abdominal pain and fever were the most common presenting symptoms in children between 2 and 5 years of age [62]. After 5 years, the classic lower urinary tract symptoms, including dysuria, urgency, urinary frequency, and costovertebral angle tenderness, are more common [62]. Regardless of age, all children should have their sacral region examined for dimples, pits, or a sacral fat pad, because the presence of these signs is associated with neurogenic bladder. In all boys, a scrotal examination should be performed to evaluate for epididymitis or epididymo-orchitis. Urine, which should be obtained before the initiation of antimicrobial therapy, can be collected by various methods. The simplest and least traumatic method is via a bagged specimen, which involves attaching a plastic bag to the perineum. Clinicians, however, are discouraged from obtaining a urine specimen in this fashion because there is an unacceptably high false-positive rate of 85% or higher [60]. The catheterized specimen is considered reliable provided that the initial portion of urine that may be contaminated by periurethral organisms is discarded. The disadvantage of urethral catheterization is that it is invasive and periurethral organisms may be introduced into an otherwise sterile urinary tract. Suprapubic aspiration is considered the gold standard for accurately identifying bacteria within the bladder. The culture information should be interpreted in the context of the clinical scenario when determining the appropriate therapy. Because urine culture typically requires at least 24 hours of incubation, urinalysis and urine microscopy are often used to guide initial empiric therapy. Under high-power magnification, the presence of bacteria represents approx A 4 imately 3 10 bacteria/mL [48]. Urine microscopy, however, cannot distinguish a uropathogen from contaminating bacteria. Hoberman and Wald [66] reported 3 that the positive predictive value of pyuria (10 white blood cells/mm) and bacteriuria is as high as 84. Certain bacteria, particularly gram-negative bacteria, reduce nitrates to nitrites. This test may produce false-negative results if it does not contain the first voided specimen, the bacteria are gram-positive organisms, or there has not been enough time for bacterial metabolism to produce nitrites. The authors argued that the use of ultrasound to identify a urinary tract malformation is minimal given the prevalence of prenatal ultrasonography in the United States. Imaging studies generally can be pursued after the resolution of the acute infection because immediate management typically is based on clinical signs and symptoms. Anti microbial therapy should be initiated promptly after a proper urine culture is obtained. In these patients, a broad-spectrum antibiotic is recommended for empiric coverage (Table 2). These patients should be managed with hospital admission, rehydration, and parenteral broad-spectrum antimicrobial therapy immediately after urine culture is obtained (Table 3). Of note, infants younger than 60 to 90 days are more likely to have their course of disease change rapidly because of their physiology and incompletely developed immune system [36,80]. Asep sis evaluation that includes a suprapubic aspirate and blood cultures should be initiated upon evaluation. Any patient with questionable compliance or difficulty with follow-up should be considered for inpatient management. In general, the combination of ampicillin or cephalosporin (eg, cefazolin) plus an aminoglyco side (eg, gentamicin) is adequate coverage for most uropathogens. Because of changing resistance patterns of uropathogens and a concern for nephrotoxicity, a single third-generation cephalosporin (eg, ceftriaxone or ceftazidime) is increas ingly being used as an alternative initial regimen [50]. The promptness of therapy for suspected acute pyelonephritis is of paramount importance, because a delay in therapy has been associated with more severe infections and worse renal damage [75,83]. Parenteral treatment is maintained until a patient is clinically stable and afebrile, generally 48 to 72 hours. At that point, the antimicrobial regimen may be changed to an oral agent based on the sensitivities of the urine culture. Numerous published studies, however, have shown resolution of symptoms and eradication of the causative agent with a 7 to 14-day course of antibiotics [53,75,84]. Alternative options for ambulatory management include outpatient parenteral therapy for patients with clinical presentations consistent with acute pyelonephri tis. Once the uropathogen is isolated in the urine culture and the antimicrobial sensitivities are finalized, children can be switched to an oral agent to complete a 10-day treatment course. Intravenous and oral formulations of fluoroquinolones have been shown to have excellent cov erage of gram-negative and -positive organisms in the urinary tract [87]. The available scientific data, however, fail to demonstrate an unequivocal association with arthropathy in the pediatric population [89,90]. In large tertiary care neonatal intensive care units, Bryant and colleagues [91] found the overall incidence of candiduria to be 0. Risk factors for the development of funguria include long-term antibiotic treatment, use of urinary drainage catheters, parenteral nutrition, and immunosuppression [92]. The clinical presentation of patients with funguria ranges from an absence of symptoms to fulminant sepsis. The urinary tract is most frequently the primary entry point but also may represent the site of disseminated infection. Consequently, the challenge for clinicians is to determine whether the presence of fungus in the urinary tract represents infection, coloni zation, or contaminant. Urine cultures with 4 more than 10 colonies/mL have been used as the criterion for therapy [94]. The presence of a positive urine culture result mandates an evaluation of the upper urinary tract with renal ultrasonography for additional foci of funguria. Investigations conducted in adult populations have shown that treatment of asymptomatic bladder infections results in poor long-term eradication rates and essentially no clinical benefit [95,96]. The removal of indwelling catheters has not been shown to clear infections reliably [48]. Symptomatic patients can be treated with bladder irrigations of amphotericin B or oral fluconazole. Although there is no consensus on optimal treatment dose or duration, amphotericin blad der irrigations consist of daily irrigations of 50 mg/L for 7 days [97] or con tinuous irrigations (42 mL/h) for 72 hours [98]. Patients with these upper tract foci of funguria should be treated with systemic therapy that consists of amphotericin B or fluconazole. In cases of obstruction, percutaneous nephrostomy is then used for drainage and potential local irrigation. Antimicrobial prophylaxis Because renal damage and scarring have been shown to occur only in the presence of infection, the goal of antimicrobial prophylaxis is to sterilize the urine [99]. The ideal prophylactic antimicrobial agent should be administered orally and achieve a therapeutic drug level in the urine while concomitantly main taining low fecal concentrations (Table 4). Similar to the selection of an antibiotic for treatment, the agent chosen for prophylaxis should be based on local antimicrobial resis tance patterns. After the treatment course for a first infection, infants or neonates should be placed on a different antimicrobial agent for prophylaxis until a thorough eval uation for an anatomic urinary tract abnormality is completed [74]. Asymptomatic bacteriuria Bacteria may be present in the urinary tract without any associated symp toms. Ultimately, there was one episode of pyelone phritis and no evidence of decreased renal function at the end of the study. Similarly, Schlager and colleagues [110] reported on asymptomatic bacteriuria in children undergoing clean intermittent catheterization. These investigators con cluded that asymptomatic bacteriuria is not associated with renal damage and the incidence of actual symptoms is low. If a child is found to have asymptom atic bacteriuria without an associated urinary malformation, then clinicians are recommended to follow-up with patients periodically without concurrent anti microbial therapy. As a result, it is difficult to determine whether an episode of cystitis will resolve without incident or result in more serious infection involving the kidney. A pediatric urology referral should be considered in children suspected of having serious sequelae of pyelonephritis, including renal abscess formation, pyonephrosis, emphysematous pyelonephritis or cysti tis, and xanthogranulomatous pyelonephritis [74,111]. Prompt recognition and treatment of upper tract infection are crucial to preventing potential irreversible renal damage. The most widely used method of 99 detecting renal scarring is Tc-labeled dimercaptosuccinic acid scintigraphy scan [69]. Smellie and col leagues [1] found renal scarring more commonly in infants and young children and less frequently in older children and young adults, which suggests that youn ger kidneys are more susceptible to damage. The incidence of hypertension in adulthood after urinary infection ranges from 7% to 17% [1,116,118]. The pathogenesis, however, remains un clear, although the renin-angiotensin system and atrial natriuretic peptide have been proposed as mechanisms. To date, no direct relationship among severity of hypertension, degree of renal scarring, and glomerular filtration rate have been established. Wennerstrom and col leagues [120] showed that glomerular filtration rate was significantly reduced in scarred kidneys during a 20-year follow-up period. In another study by Jacobson and colleagues [116], 30 children with nonobstructive focal renal scarring were followed for 27 years. Ultimately, 3 patients with bilaterally scarred kidneys developed end-stage renal disease. Chil dren, however, have a wide variety of clinical presentation, ranging from the asymptomatic presence of bacteria in the urine to potentially life-threatening infection of the kidney. The indwelling ureteric stent: a friendly procedure with unfriendly high morbidity. Bacteriology of urinary tract infection associated with indwelling J ureteral stents. Effect of a single-use sterile catheter for each void on the frequency of bacteriuria in children with neurogenic bladder on intermittent catheterization for bladder emptying. Newborn circumcision decreases incidence and costs of urinary tract infections during the first year of life. Genetic evidence supporting the fecal-perineal urethral hypothesis in cystitis caused by Escherichia coli. Clonal diversity of Escherichia coli colonizing stools and urinary tracts of young girls. Urologic diseases in North America Project: trends in resource utilization for urinary tract infections in children. Incidence rate of first-time symptomatic urinary tract infection in children under 6 years of age. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs.
Not only do male obstetrician-gynecologists feel at times that they are losing ground diabetes diet pregnant metformin 850 mg on line, but some recruiters from private practice groups have be gun discriminating against male physicians diabetes mellitus vs type 2 generic metformin 850mg amex. Assuming that women prefer a fe male obstetrician-gynecologist managing diabetes and hypertension purchase discount metformin online, these practices aggressively seek female residents diabetes insipidus traumatic brain injury buy metformin in united states online. They want to balance their male-dominated staff with female obstetrician-gyne cologists diabetic pills buy 500 mg metformin mastercard, creating a dramatically changed workforce type 1 diabetes quick reference order metformin with visa. As a result, many qualied male doctors struggle to secure their preferred career. In fact, one study found that 26% of graduating male residents reported difficulty in nding a job, com pared to 17% of female residents. The idea that female patients feel more comfortable with a female obstetrician-gynecologist is completely erroneous. In a recent survey of obstetric patients during their postpartum hospital stay, the majority (58%) had no preference for the gender of their obstetrician; 34% preferred female physi cians and 7% indicated a desire for a male doctor. Men who cultivate traditionally female skills, particularly empathy and good communication, can thrive as obstetrician-gynecologists. The current medicolegal climate of our society, with its get-rich quick incentives, makes obstetrics and gynecology a high-risk specialty. In fact, most medical students considering this specialty are especially concerned about the daily potential litigation. In light of this ever-present malpractice menace, obstetrician-gynecologists must be passionate about their careers and provide outstanding patient care. In many instances, the threat of lit igation encourages the development and training of better physicians. If you look at all the statistics and numbers, obstetrician-gynecologists have the highest incidence of lawsuits throughout their careers. Since the 1950s, the number of malpractice claims led against obstetrician-gynecologists has in creased nearly 15% every year. More than half of all claims were dismissed, settled without payment, or won by the physician. Due to unaffordable liability insurance premiums (or even the inability to obtain insurance) many physicians have curtailed their services. They are forced to reduce the number of deliveries they perform, cut back on high-risk patients, and even stop some sur gical services. This loss of access to prenatal and delivery care particularly affects women in rural and inner-city communities, which are typically underserved. As a result, many obstetricians are banning together in various states to pass tort re form bills that cap the restitutions patients can gain. In California, physicians lob bied to enact a series of reforms that curbed soaring liability premiums, stopped physicians from leaving the state, and prevented the decrease in availability of care. The 50-year challenge of malpractice will continue to be an important is sue for future obstetrician-gynecologists. Many med ical students wonder about the role of family practitioners and midwives, how ever, as providers of pregnancy-related care. A midwife (meaning with a woman) provides prenatal care, attends childbirth, manages her clinic patients during la bor and delivery, and supervises the general care of women and children directly after birth. As advanced degree registered nurses, nurse midwives have completed an accredited midwifery program and passed the certication examination. Nurse midwives, how ever, attend only about 9% of vaginal births in the United States. As such, their professional relationship should always remain collegial and cooperative. There are apeutically, they are experts at high-risk currently 254 accredited pro deliveries, abortions, laparoscopy, fetal grams. Gynecologic Oncology Instead, residents immediately Roughly 15% of all cancers found in begin surgical training in obstet women involve tumors of the reproduc rics and gynecology. This area of specialization fo quired to prove competency in all cuses on the medical and surgical care of surgical and obstetric proce women with malignancies arising in the dures. The typical monthly rota reproductive system: ovarian, uterine, tions include labor and delivery, cervical, vulvar, and vaginal cancer. They are at least 6 months of outpatient skilled pelvic surgeons who use the latest rotations. About 10% of residents techniques in radical surgery, chemother continue their training in fellow apy, and radiation treatment. Gynecologic oncologists are sup ported by a multidisciplinary team of medical oncologists, radiation oncologists, and gynecologic pathologists who collaborate to provide optimal care. Their practice also extends to the treatment of hormonal and repro ductive disorders affecting women, children, men, and mature women. Repro ductive endocrinologists gain special competence in advanced microsurgical pro cedures, such as reversal of tubal ligation, treatment with fertility drugs, and methods of assisted reproduction (in vitro fertilization and insemination). Female Pelvic Medicine and Reconstructive Surgery As women age, a history of multiple deliveries and other forms of strain may cause the musculature supporting the pelvic contents to slowly weaken. This can lead to disorders such as urinary incontinence or a prolapsed bladder, uterus, or vagina. To correct pelvic oor dysfunction, women should seek out specialists in female pelvic medicine and reconstructive surgery. Also known as urogynecology, this advanced surgical subspecialty remains on the cutting edge of medicine. It integrates the elds of urology and obstetrics-gynecology in the operating room. To diagnose pelvic prolapse and female voiding dysfunction, these physicians have special expertise in clinical evaluation, cystoscopy, and analysis of urody namic testing. Because this is a surgical fellowship, specialists in pelvic medicine perform many reconstructive operations to correct pelvic oor dysfunction. Despite its seemingly specialized nature, obstetrics and gynecology provide much diversity and variety. Because of the diverse age of patients, your scope of practice can range from broad (primary ambulatory care) to very narrow (concentration in an area of spe cialization). With so many paths available within this one specialty, there is no limit to what you may be able to offer to obstetrics and gynecology. After all, a single obstetrician or gynecologist cannot provide for all of the needs of a woman. The positive interactions between generalists and subspecialists allow for the highest quality of care for women of all ages. Despite the rigorous lifestyle and the pressure of handling the high-risk responsibility, there are lots of rewards. Future obstetricians-gynecologists will be part of a group of caring, competent, and conscientious doctors who strive for the best patient care for women. Kelly Oberia Elmore is a resident in obstetrics and gynecology at the Naval Medical Center in San Diego. Primary care in obstetrics and gynecology residency edu cation: A baseline survey of residentsperceptions and experience. Families with inher ited congenital anomalies, such as Apert or Crouzon syndrome, may have multi ple generations followed by the same sur geon. Similarly, many problems in the upper extremity mandate a careful, staged approach to treatment. For ex ample, if a man loses his thumb in a farm ing accident, he will need a procedure to achieve closure of his initial wound. He will require reconstruction to provide him with useful thumb function, which can sometimes take the form of a toe-to thumb transfer. The surgery itself is quite involved and rehabilitation is certainly a long-term endeavor. Likewise, patients with facial paralysis (such as with Bell palsy) or brachial plexopathies may require multiple therapeutic procedures over several years. The training is intense, espe cially during the core surgery years, and the clinical component of most cate gorical plastic surgery programs lasts 6 years. Most plastic surgeons, including this author, have participated in operations that lasted more than 24 hours. Not only can these pro cedures be long, but the anastomosis of small vessels can sometimes be quite challenging. Mental disorders (particularly depression and alcohol abuse) rank among 7 out of the top 10 leading causes of disability in developed countries. Psychiatrists derive a great deal of personal fulllment in actively helping patients who have debilitating mental disorders. Treatment with drugs usually ends up being long term, and there are few actual cures. Unlike cases of physical disease, when there is successful treatment in psy chiatry, the credit is usually given to the patient instead of to the drug or psychi atrist. Long ago, mentally ill patients were often placed in public institutions be cause they were thought to be harmful to themselves or to others. These agents not only treat depression, but also help manage cases of panic dis order, obsessive-compulsive disorder, and social phobia. Antipsychotic medica tions also underwent a revolution with the introduction of atypicals (like Risperi done, olanzapine, and quetiapine), which have fewer adverse reactions. Psychopharmacology involves more than just antidepressant, antipsychotic, and anticonvulsant medications. Of course, it is specic to urologic care, but taking care of children is different than taking care of adults and these differences must be learned. Fluid management is differ ent, medicine dosing is different, comorbidities are different, and in general, kids have much higher physiologic reserve and therefore can look well up until the moment they crash. Neurology is a eld that plays into the urology database, in that people with spinal cord injuries, congenital or acquired, inevitably have bladder dysfunction. Having a working knowledge of the nervous system, particularly as it relates to the pelvic organs, becomes paramount in treating a neurogenic bladder. Finally, it is essential for urologists to have an understanding of the radio logic imaging that a urologic patient may undergo. As with any surgical specialty, diagnosis is often predicated completely on what the scan looks like. For example, if a man with testicular pain and no palpable mass is sent for a scrotal ultrasound, and a small testicular mass is noted, he will immediately get a workup for testic ular cancer. Based on the ultrasound ndings alone, he may require counseling for surgical excision. Based on these ndings alone, she is diagnosed with probable renal cell carcinoma and offered surgical excision. Renal function for patients with an atrophic looking kidney can be assessed using nuclear medicine. For example, a dimercaptosuccinic acid scan, a radioisotope that binds to renal parenchyma, gives a sense of how well the kidneys are ltering blood, the left compared to the right. Medical students considering a career in urology must accept that this spe cialty is denitely still a surgical eld. In some European countries, urology has been divided into two tracts: operative urology and office urology. In the United States, some think that urology is headed toward that same division. In the mean while, however, urologists still manage both sides of the operating room. In re ality, a community practice urologist may opt to refer all big open cases to an aca demic center. This referral pattern has evolved due to the amount of work these bigger cases entail and the poor reimbursement standards. This means that a typical community urologist only performs straightforward open surgery. Ritter this eBook is for the use of anyone anywhere at no cost and with almost no restrictions whatsoever. You may copy it, give it away or re-use it under the terms of the Project Gutenberg License included with this eBook or online at