Shaon Sengupta, MBBS, MPH
- Attending Neonatolgist, CHOP & Instructor, Penn
- Research Interests: Circadian underpinnings of lung inflammation

https://www.med.upenn.edu/fitzgeraldlab/personnel.html
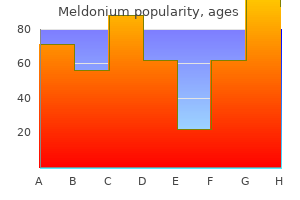
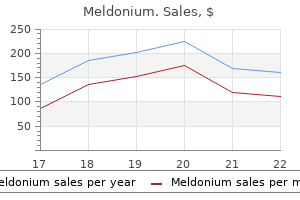
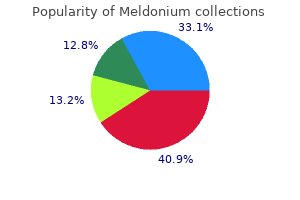
Cyclophosphamide and sequential cisplatin for advanced seminoma: long-term followup in 52 patients medicine neurontin order meldonium no prescription. Chemotherapy of metastatic seminoma: the Southeastern Cancer Study Group Experience treatment of lyme disease order meldonium 500mg without a prescription. A Scottish national audit of current patterns of management for patients with testicular non seminomatous germ-cell tumours medicine you can take while breastfeeding meldonium 500 mg overnight delivery. A randomized trial of standard chemotherapy v a high-dose chemotherapy regimen in the treatment of poor prognosis nonseminomatous germ-cell tumors treatment 1st 2nd degree burns order genuine meldonium line. The National Cancer Data Base report on patterns of care for testicular carcinoma medications related to the female reproductive system order cheap meldonium online, 1985 1996 medicine hat lodge 250 mg meldonium for sale. Adjuvant radiation versus observation: a cost analysis of alternate management schemes in early-stage testicular seminoma. Management preferences following radical inguinal orchidectomy for Stage I testicular seminoma in Australasia. Survey of radiation oncologists: Practice patterns of the management of stage 1 seminoma of the testis in Canada and a selected group in the United States. Treatment outcome of patients with brain metastases from malignant germ cell tumors. Th e incidence ofattributes used to define indications forradioth erapy K ey Populationor A ttribute Proportionof Q uality of R eferences N otes subpopulationof populationwith information interest th is attribute A A llregistry cancers A lllymph omas 0. The use of chemotherapy alone is not currently recommended by the guidelines, although it may need to be considered if there is a young female who will require her breast to be irradiated. It should not be excluded if there is a bulky mediastinal mass but only if bilateral axilla require treatment. Patients over the age of 60 are less likely to be fit enough to tolerate and complete radical treatment, and will not be considered for bone marrow transplant for an incomplete response or on relapse. It was therefore decided to split the group by age at this stage of the radiotherapy utilisation tree. Because the Swedish study separates the patients by stage and age, this data will be used in the analysis. Guidelines recommend that radiotherapy should be considered for all patients who achieve a partial response to chemotherapy to improve local control rates(3) (38). Radiotherapy to sites of non-bulky disease after a complete response to chemotherapy is not routinely recommended. Bone Marrow Transplant: Indications for bone marrow transplant include progressive disease on initial conventional chemotherapy, or relapse within 1 year of initial treatment (2). Not all of these patients will be suitable for transplant, with the actual percentage of patients transplanted being 32% (14). The role of total body irradiation conditioning prior to transplant remains controversial. No Bone Marrow Transplant: this group have chemoresistant disease, have relapsed greater than 1 year after initial treatment or are considered inappropriate for bone marrow transplant. Single institution case series of radiotherapy alone for relapsed disease report relapse-free survivals of 30-48% (41). Relapse after bone marrow transplant: Forty-five percent of patients relapse after bone marrow transplant, usually at sites of previous disease (39). These patients should now have radiotherapy considered as part of their further management. The role of total body irradiation conditioning prior to transplant remains controversial. If not fit enough for treatment with radical intent they will still benefit from palliative radiotherapy to sites of bulky disease. Although this is lower than the younger population the rate of relapse is similar, at 26%. The response reflects the inability to administer certain drugs and adequate doses to the older population. Treatment of relapsed disease in this older population, if considered appropriate, is with second line chemotherapy for those who are fit enough. Radiotherapy is considered for limited nodal relapse, symptomatic nodal or extranodal disease if unfit for chemotherapy and as consolidation after a second complete response. Stage distribution at diagnosis, is classified using the Ann Arbor staging system which categorises stage using number of sites of nodal or extranodal involvement above and below the diaphragm, and the presence or absence of well-defined generalised "B" symptoms. In the Working Formulation three groups are identified as low, intermediate and high grade. Response rates can vary from 35-100%, although most report complete response of about 80%. I have selected the larger reports from 2 international groups rather than single institutional case series. Those who do not achieve a complete response are likely to be offered alternative treatment with radiotherapy. One study who followed 40 cured patients of which 10% have relapsed after a median follow-up of 2 years (26). In keeping with guidelines curative or palliative radiotherapy is indicated for these patients (4-6). Reports from multi-institutional databases, which is the highest ranking evidence, range from 38-65%. Two other recent reports on the use of chemotherapy for advanced disease, although lower ranking, also report on response rates of 65%. This has been used in the analysis although a sensitivity analysis will be performed. Treatment for relapse is heterogeneous, with most patients receiving further chemotherapy. Two single institutions report on response rates to second line chemotherapy of about 70% overall. This proportion, which included patients treated with Fludarabine and stem cell transplant, will be used (32;46). Guidelines recommend palliative radiotherapy for symptomatic disease or for residual masses after chemotherapy. The patients who did not respond to or achieved an incomplete response to second line chemotherapy should be considered for palliative radiotherapy. This group have required treatment for symptoms, but have failed to respond to chemotherapy. Prior to being considered for palliative radiotherapy they are likely to be treated with an alternative chemotherapy regimen. Two single institutions report on response rates to second line chemotherapy of about 70% overall. This proportion, which included patients treated with Fludarabine and stem cell transplant, will be used (32;46). Guidelines recommend palliative radiotherapy for symptomatic disease or for residual masses after chemotherapy. The patients who did not respond to or achieved an incomplete response to second line chemotherapy should be considered for palliative radiotherapy. Reports from multi-institutional databases, which is the highest ranking evidence, range from 38-65%. Two other recent reports on the use of chemotherapy for advanced disease, although lower ranking, also report on response rates of 65% (22-25). This has been used in the analysis although a sensitivity analysis will be performed. Treatment for relapse is heterogeneous, with most patients receiving further chemotherapy. Two single institutions report on response rates to second line chemotherapy of about 70% overall. This proportion, which included patients treated with Fludarabine and stem cell transplant, will be used (32;46). Guidelines recommend palliative radiotherapy for symptomatic disease or for residual masses after chemotherapy. The patients who did not respond to or achieved an incomplete response to second line chemotherapy should be considered for palliative radiotherapy 26. This group have required treatment for symptoms, but have failed to respond to chemotherapy. Prior to being considered for palliative radiotherapy they are likely to be treated with an alternative chemotherapy regimen. Two single institutions report on response rates to second line chemotherapy of about 70% overall. This proportion, which included patients treated with Fludarabine and stem cell transplant, will be used (32;46). Guidelines recommend palliative radiotherapy for symptomatic disease or for residual masses after chemotherapy. The patients who did not respond to or achieved an incomplete response to second line chemotherapy should be considered for palliative radiotherapy. Elderly patients or patients considered unfit for chemotherapy would be considered for radiotherapy with either curative or palliative intent (47). Guidelines recommend radiotherapy for bulky disease (4), however the proportion of patients who present with advanced in the chemotherapy trials for the advanced intermediate group. Most population based data includes heterogeneous groups with a small proportion being treated for early disease and some with radiation only. In a population based study the complete response rate for advanced intermediate disease was 44%. A higher response was documented in patients under the age of 70 years (51%) when compared to patients over 70 years (33%) (28). Younger patients who relapse after a complete response are likely to be considered for high dose chemotherapy and bone marrow transplant. This data could not be identified and it was therefore decided to split the tree by age at this point. This study randomised patients to high dose treatment after a response to second line conventional chemotherapy. Radiotherapy was recommended in both arms of the study to sites of bulky disease >5cm or T3/T4 extranodal disease (30%). The addition of radiotherapy reduced the incidence of local recurrence observed in both the transplant and non-transplant arm (34). Relapse at the primary site was recorded in 50% of patients treated with chemotherapy alone compared to 26% when radiotherapy was also delivered. From this information radiotherapy should be considered to initial sites of disease in patients who relapse with these indications. Intermediate grade lymphoma, treatment for relapse after a complete response, > 70 years: Forty-four percent of patients >70 years subsequently relapsed (28). Treatment at this time will be individualised depending on the ability of the patient to tolerate further chemotherapy. Greil has published a review article on management strategies of lymphatic neoplasms in the elderly (51). Although initial curative treatment is warranted he identified that a significant proportion of elderly patients received reduced dose chemotherapy and were unable to adequately tolerate treatment. Their chance of receiving adequate treatment with chemotherapy alone on relapse is unlikely. These patients should be considered for palliative radiotherapy in the presence of bulky disease. Both a population based study and a multi institutional report identify similar proportions of elderly and young patients presenting with bulk disease. It was therefore concluded that a similar proportion of elderly patients would relapse with bulky disease as the younger trial group (34). This proportion (30%) was included in the analysis to distinguish a proportion of patients who should receive radiotherapy. Intermediate grade lymphoma, incomplete response to chemotherapy, > 70 years: In a population-based study 59% of patients who did not obtain a complete response to first line chemotherapy were under the age of 70 years (28). Guidelines would recommend radiotherapy to either initial sites of bulky disease or residual masses. Guidelines recommend that they should be treated on leukaemic protocols, which include prophylactic cranial irradiation. For unfit patients, palliative radiotherapy to symptomatic lesions is recommended. Optimal Radiotherapy Utilisation Rate and Sensitivity Analysis the proportion of lymphoma patients in whom at least one course of radiotherapy is indicated is 65%, based on guideline recommendations. There are several data elements where there was uncertainty because of different proportions reported in the literature. To assess the impact that these uncertainties have on the overall estimate of the need for radiotherapy in all lymphoma patients, a one way sensitivity analysis was performed for each of the variables and the impact that these variables have on the overall results is illustrated by a tornado diagram. The graph shows that the proportion of lymphoma patients that should receive radiotherapy based on evidence and incidence of attributes for radiotherapy was 65-66%. As lymphoma represents 4% of all reported malignancies, the proportion of lymphoma patients where radiotherapy is indicated represents 2. Mucosa-associated lymphoid tissue lymphoma is a disseminated disease in one-third of 158 patients analysed. Eradication of Helicobacter pylori and stability of emissions in low-grade gastric B-cell lymphomas of the mucosa-associated lymphoid tissue: results of an ongoing multicenter trial. Cure of Helicobacter pylori infection and duration of remission of low-grade gastric mucosa associated lymphoid tissue lymphoma. Prognosis of follicular lymphoma: a predictive model based on a retrospective analysis of 987 cases.
Power analysis was based on expected 10% eradication in the absence of treatment and 50% eradication with treatment symptoms yeast infection women 500 mg meldonium mastercard. In this analysis medications and mothers milk 2014 500mg meldonium, the planned sample was a maximum of 50 patients (n = 25 per group) symptoms 20 weeks pregnant safe 250 mg meldonium, which leads to 94 medicine 512 buy meldonium 500 mg with visa. A total of 46 patients completed the study at time of analysis with the remaining planned to conclude in February 2019 treatment 911 order 500mg meldonium free shipping. Method: Guided by a Global Expert Advisory Panel with patient and clinical representation symptoms congestive heart failure order 250mg meldonium visa, the study included a literature review of global trends in incidence, mortality, and survival of ovarian cancer, qualitative interviews with women and clinicians in 16 countries, and an online survey available in 15 different languages (open March to May 2018). Given global 5-year prevalence, results in this survey achieve a confidence level of 95% with a confidence interval of 2. Results: With global incidence set to rise by 55% to 371,000 a year, 5-year survival rates of less than 50%, and 15% dying within 2 months of diagnosis, urgent action is required to improve survival. More than two-thirds of woman had not heard of ovarian cancer or knew anything about it prior to their own diagnosis. Ninety percent of respondents reported experiencing multiple symptoms prior to their diagnosis regardless of type. There were wide variations between countries and in the subsequent time to diagnosis. There were wide levels of variation in genetic testing, both pre and post-diagnosis, by country (9. Of those women with 2 or more relatives with ovarian cancer, 80% had not had genetic testing prior to their diagnosis. Clinicians indicate that access to specialist treatment in high-volume centers varies widely by country and region. Conclusion: Low level of awareness of ovarian cancer is a global problem resulting in delays in women seeking medical attention and being diagnosed. Women are potentially missing out on new targeted treatments for ovarian cancer, and family members are unaware of risk because of variable rates of genetic testing. Ensuring that all woman have access to specialist 58 treatment is a vital step to improving outcomes worldwide. In phase 2 an online survey was publicized through various online and print channels throughout the period of both phase 1 and phase 3. Results: Significant numbers experienced, or continue to be affected by, several, often complex, long-term consequences of their diagnosis and treatment including the following: 86% experienced at least 1 physical long-term consequence; 63% experienced 3 or more; and 24% experienced 6 or more. Of which 67% experienced changes in their sex life; 64% suffered fatigue; 54% bowel difficulties; 54% urinary difficulties; 44% lymphedema; and 60% said employment changed due to their treatment. High numbers hadn?t sought medical advice about the difficulties experienced including 39% who had changes to bowel function and 42% urinary function; 59% with negative changes to or a complete loss of sex life; 44% affected by pain and/or fatigue; and only 32% who have experienced reduced, or even lost, fertility talked to a physician. It highlights that high numbers of women are affected by multiple negative consequences of their treatment and demonstrates their complex, wide-ranging needs. Women presenting with problems are not being referred or diagnosed correctly, often being told there is nothing that can be done and being left to self-manage life-changing symptoms without the right diagnosis. There needs to be increased understanding and awareness of the long-term consequences across healthcare, and women need to be empowered to feel they are able to ask questions, ask for help, and be confident their concerns will be recognized and addressed. Patient characteristics, methods of chemotherapy and radiotherapy, late adverse events, and oncologic outcomes were analyzed. Kaplan-Meier life table analysis and the log rank test were used to assess the survival rate. Median age was 58 years (range 24?58 years), and median tumor diameter was 50 mm (range 11?120 mm). Results: We extracted selected populations using propensity score matching with 1:1 ratio. In multivariate analysis, clinical stage was still a significant risk factor after adjusting for the other clinical parameters. Over 97% reported no pain or least amount of pain (scores 1?3) during treatment, and 99% were highly satisfied (scores 7?9) with and willing to recommend the treatments. Whatever treatment method is used, however, the high rate of recurrence warrants long-term follow-up surveillance. Conclusion: In our nationwide population-based cohort study, metformin reduced all-cause mortality in ovarian cancer when used in long-term duration. Whether metformin reduces deaths because of ovarian cancer itself needs further investigation. Poster Session Sunday, March 17, 2019 Basic and Translational Science 1101 Poster Session Biomarker panel for early detection of endometrial cancer in the prostate, lung, colorectal, and ovarian cancer screening trial C. We sought to identify early detection biomarkers for endometrial cancer using prediagnostic serum. One hundred and twelve incident endometrial cases were matched 1:1 with controls based on age, race, study site, year of blood draw, and year of randomization. Prediagnostic serum was immunodepleted of high-abundance proteins and digested with sequencing-grade porcine trypsin via pressure cycling technology. Quantitative proteomics and phosphoproteomics were performed using high-resolution liquid chromatography tandem mass spectrometry and highly multiplexed isobaric mass-tag combined with basic reversed-phase liquid chromatography. A set of proteins able to predict cancer status was identified with an integrated score assessed by receiver operator curve analysis. There were 47 differentially abundant proteins between cases and matched controls (P < 0. Protein alterations with high predictive potential were selected by regression analysis and compiled into an aggregate score to determine the ability to predict endometrial cancer. An integrated risk score of six proteins (complement factor B, serotransferrin, catalase, proteasome subunit beta type-6, beta-2-microglobulin, and protocadherin-18) was directly related to disease incidence in cases with blood draw? The integrated score was able to distinguish cases from controls with an area under the curve of 0. Validation is needed to evaluate whether this test can improve prediction or detection of endometrial cancer among postmenopausal women. Unpaired two-tailed Student t test was employed to determine statistical significance of results. Method: All newly diagnosed patients with suspected ovarian cancer who were undergoing primary cytoreductive surgery at our center from December 2017 to July 2018 were offered to participate in the study. Results: Baseline imaging of tumor blood vessels was successful in all six patients with fluorescein present within the vasculature. This obstacle was overcome in the remaining four out of five patients with use of the Thompson retractor rail clamps and two angled arms while placing the mobilized omentum over the arms for tissue stabilization. Following adoption of the Thompson retractor technique, four patients were successfully observed with at least 15 minute observation time and minimal movement. There were no reported patient adverse events or toxicity other than temporary fluorescein-related urine color changes. This new in vivo technique will allow for future studies to examine real-time characterization of tumor vessels, immune cell trafficking, anti-angiogenic therapy, and chemotherapy delivery. An "immune signature," previously validated from bulk sequencing, was used to further define immune subsets of cells. Results: Transcript expression was characterized for an average of 1,522 (range 1,054?2,368) cells per sample, with a mean of 176,433 (range 98,436?244,591) reads per cell in the seven sites. Based on differentially expressed gene analysis, we defined cell clusters as epithelial, stromal, immune, or endothelial. Twenty-four tumor cells were isolated from each tumor at the time of primary debulking using Fluidigm C1 and subsequent whole exome-sequencing. Variant calling was performed with FreeBayes, and variants were annotated with Annovar for review by a molecular pathologist. Results were compared to parallel germline medical Exome sequencing to discriminate somatic versus germline origin in the single-cell data. Results: Four patients (two high-grade serous, one mucinous borderline, and one mucinous carcinoma) had 24 cells each captured. Comparison of single-cell and high-depth bulk sequencing will characterize the analytic performance of each. Conclusion: Subclonal mutational heterogeneity may drive resistance to standard therapy and promote disease recurrence. We demonstrate that potentially pathogenic mutations in these four patients show evidence for subclonal heterogeneity in single cell Exome-sequencing data. Landmarks for proving structure consisted of identifying the iliac vessels in the pelvic sidewall and the tubal vessels located posterior and parallel to the fallopian tubes. Pressure was applied to three or more regions of the abdominal surface to achieve bowel repositioning in order to assist visualizations. Results: Visualization of both ovaries decreased with age with only 50% of patients aged 75?76 years having both ovaries identified (dashed line in Figure 1). A crossover point is noted for women in their mid-80s where nonvisualization of both ovaries surpassed visualization. Both ovaries were visualized in ~93% of premenopausal women and ~69% of5 postmenopausal women. Furthermore, the effect of dinaciclib resulted in persistent tumor inhibition in vivo, while carboplatin and paclitaxel combined induced only transient suppression of tumor growth. Dinaciclib induced 68% tumor reduction from vehicle control compared with 12% tumor reduction induced by chemotherapy (paclitaxel plus carboplatin). Tumor growth inhibition by dinaciclib was 56% superior compared to the standard of care. Statistical analyses showed that dinaciclib versus vehicle effect was significant (P = 0. We also found an additive or synergistic effect in combination with everolimus in three of four cell lines tested. As a novel therapeutic approach for the prevention of ovarian cancer metastasis, we aimed to modulate the expression and activity of gal-3 and alter the metastatic efficiency and organotropic behavior of cells in vitro and in vivo. Metastatic behavior was observed and survival data were collected for both experiments. Data were analyzed using unpaired t tests and Kaplan-Meier survival analyses with log rank tests. These results are the basis for further studies to assess gal-3 inhibition for the blockade of metastatic invasion and colonization in ovarian cancer. Method: Patients treated between August 2012 and July 2015 for cervical carcinoma with definitive chemoradiation were identified. Toxicities were assessed during weeks 1?6 of concurrent external beam radiation and chemotherapy. The majority of the patients were Hispanic (n = 83, 69%), followed by African-American (n = 30, 25%), and Caucasian (n = 8, 6%). The most common grade 4 toxicity was lymphopenia, experienced by 36% of patients (n = 44). Continued work is needed to explore treatments that do not deplete lymphocyte count during cancer treatment. Mutational signatures were defined using deconstructSigs, and results were correlated with clinicopathologic and genomic data. Adhesion and invasion were assessed by laminin and wound healing assays, respectively. At the same doses of treatment, both drugs caused an increase in G2 cell cycle arrest (P < 0. Hypersensitivity reactions to Cremaphor are encountered in 30%?45% of treated patients. Results: For the 44 paired samples analyzed, median age at diagnosis was 59 (range 35?77) years. The majority of patients had advanced-stage disease (34, 77%) with serous histology (31, 30%). Patients received a median of 3 treatment regimens (range 1?13) between paired samples. Repeat tumor testing may be useful in the determination of eligibility for molecularly targeted clinical trials. Cell surface protein enrichment was performed; median log2 ratios for each protein were calculated; and volcano plots were generated using a significance of log2 ratio >1 or <? Patient characteristics were abstracted and verified by two independent reviewers. Method: A registry of biobanked specimens at our institution was queried for diagnosis of serous ovarian cancers from 2006 to 2009. Medical records were reviewed and demographic, surgical, and pathological variables collected. Comparisons of groups used log rank tests and Cox proportional hazards adjusted for age. There were no significant differences in demographic, surgical, or pathologic factors between groups. This study is an exploratory analysis investigating the presence of immune checkpoints in endometrial cancer that could allow for development of combination immune therapies. Recurrent disease was not associated with significant differences in immune checkpoint expression. After a week, mice underwent a second bleed and bioluminescent imaging to verify tumor engraftment. Samples were randomized 2:1 to training and testing sets, and then a neural network was created and employed to differentiate samples from tumor-bearing or naive mice. The neural network analysis was a more sensitive predictor of tumor presence than bioluminescent imaging alone. The algorithm identified the presence of cancer with an area under the curve of 0. Cumulative 5-year survival was calculated by the Kaplan-Meier method and analyzed by the log rank test. Results: Of the 60 patients, 90% were black, 55% between ages 30?55 years, and 40% older than 55 yeas. Thirty-three patients had poorly, 20 moderately, and 7 well-differentiated tumors. At 5-year follow-up, 14 patients died of disease, 40 were alive, and 6 lost to follow-up; 12 of the 60 patients recurred.
The sufix m medicine 1900 best meldonium 250mg, in parentheses medicine river animal hospital buy discount meldonium, is used to indicate the presence of multiple primary tumours at a single site treatment under eye bags buy 250 mg meldonium overnight delivery. The y categorization is not an estimate of the extent of tumour prior to multimodality therapy medicine review meldonium 250mg low cost. Recurrent tumours medicine xanax buy 250 mg meldonium with amex, when classified afer a disease free interval medications 4h2 buy discount meldonium 250 mg line, are identified by the prefix r. Pn Perineural Invasion PnX Perineural invasion cannot be assessed Pn0 No perineural invasion Pn1 Perineural invasion Residual Tumour (R) Classification* the absence or presence of residual tumour afer treatment is described by the symbol R. They can be supple mented by the R classification, which deals with tumour status afer treatment. It reflects the efects of therapy, influences further therapeutic procedures, and is a strong predictor of prognosis. For purposes of tabulation and analysis it is useful to condense these categories into groups. The stage adopted is such as to ensure, as far as pos sible, that each group is more or less homogeneous in respect of survival, and that the survival rates of these groups for each cancer site are distinctive. For pathological stages, if suficient tissue has been removed for pathological examination to evaluate the highest T and N categories, M1 may be either clinical (cM1) or patho logical (pM1). However, if only a distant metastasis has had microscopic confirmation, the classification is pathological (pM1) and the stage is pathological. In this edition the term stage has been used as defin ing the anatomical extent of disease while prognostic group for classifications that incorporate other prognostic factors. Historically, age in diferentiated thyroid cancer and grade in sof tissue sarcoma are combined with anatomical extent of disease to determine stage, and stage is retained rather than prognostic group in these two sites. Prognostic Factors Classification Prognostic factors can be classified as those pertaining to . Anatomic extent of disease: describes the extent of dis ease in the patient at the time of diagnosis. These can be: predictive factors prognostic factors companion diagnostic marker. These can be demographic factors, such as age and gender, or acquired, such as immunodeficiency and performance status. This decision has stemmed from the lack of an international standard staging system for many paediatric tumours. To enable stage data collection by pop ulation-based cancer registries there needs to be agreement on cancer staging. Recognition of this led to a consensus meeting held in 2014 and resulted in the publication of rec ommendations on the staging of paediatric malignancies for the purposes of population surveillance. This has resulted in the International Histological Classification of Tumours, which contains, in an illustrated multivolume series, definitions of tumour types and a proposed nomenclature. Paediatric cancer stage in population based cancer registries: the Toronto consensus principles and guidelines. Direct extension of the primary tumour into lymph nodes is classified as lymph node metastasis. The following are the procedures for assessing T, N, and M categories: T categories Physical examination, imaging, endoscopy, and/or surgical exploration N categories Physical examination, imaging, endoscopy, and/or surgical exploration M categories Physical examination, imaging, and/or surgical exploration Anatomical Subsites 1. In a few patients, however, multiple microscopic examina tions of pleural (pericardial) fluid are negative for tumour, and the fluid is non-bloody and is not an exudate. Where these elements and clinical judgment dictate that the efusion is not related to the tumour, the efusion should be excluded as a staging descriptor. Three of these nodes stations should be mediastinal, including the subcarinal nodes and three from N1 nodes/stations. If all the lymph nodes examined are negative, but the number ordinarily examined is not met, classify as pN0. This is based on the evidence acquired before treatment, supple mented or modified by the additional evidence acquired from surgery and from pathological examination. The pathological assessment of the primary tumour (pT) entails a resection of the primary tumour, or biopsy adequate to evaluate the high est pT category. Removal of nodes adequate to validate the absence of regional lymph node metastasis is required for pN0. The pathological assessment of distant metastasis (pM) entails microscopic examination. Pathologic staging depends on the proven anatomic extent of disease, whether or not the primary lesion has been completely removed. If a biopsied primary tumour technically cannot be removed, or when it is unreasonable to remove it, the criteria for pathologic classification and staging are satis fied without total removal of the primary cancer if: a) biopsy has confirmed a pT category and there is microscopical con firmation of nodal disease at any level (pN1-3), b) there is microscopical confirmation of the highest N category (pN3), or c) there is microscopical confirmation of pM1. General Rule 3 states that clinical and pathological data may be combined when only partial information is available in either the pathological classification or the clinical classifi cation. Impact of genetic, clinical and radiologic advances since the 2004 classification. T1 Tumour 3 cm or less in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bron chus. The uncommon superficial spreading tumour of any size with its inva sive component limited to the bronchial wall, which may extend proximal to the main bronchus, is also classified as T1a. T1mi Minimally invasive adenocarcinoma T1a Tumour 1 cm or less in greatest dimension T1b Tumour more than 1 cm but not more than 2 cm in greatest dimension T1c Tumour more than 2 cm but not more than 3 cm in greatest dimension T2 Tumour more than 3 cm but not more than 5 cm; or tumour with any of the following features. In a few patients, however, multiple microscopic exami nations of pleural (pericardial) fluid are negative for tumour, and the fluid is non-bloody and is not an exudate. Where these elements and clinical judg ment dictate that the efusion is not related to the tumour, the efusion should be excluded as a stag ing descriptor. M1b Single extrathoracic metastasis in a single organ and involvement of a single distant (non-regional) node M1c Multiple extrathoracic metastases in one or several organs T Classification 1. Invasion of visceral pleura (T2) is defined as invasion beyond the elastic layer including invasion to the visceral pleural surface. The use of elastic stains is recommended when this feature is not clear on routine histology. Tumour with direct invasion of an adjacent lobe, across the fissure or by direct extension at a point where the fissure is deficient, should be classified as T2a unless other criteria assign a higher T category. Vocal cord paralysis (resulting from involvement of the recurrent branch of the vagus nerve), superior vena caval obstruction, or compression of the trachea or oesophagus may be related to direct extension of the primary tumour or to lymph node involvement. If associated with direct extension of the primary tumour a classification of T4 is recommended. If the primary tumour is peripheral, vocal cord paralysis is usually related to the presence of N2 dis ease and should be classified as such. Intrapericardial portions of the superior and inferior right and lef pulmonary veins Invasion of more distal branches does not qualify for clas sification as T4 6. The designation of Pancoast tumour relates to the symp tom complex or syndrome caused by a tumour arising in the superior sulcus of the lung that involves the inferior branches of the brachial plexus (C8 and/or T1) and, in some cases, the stellate ganglion. Some superior sulcus tumours are more anteriorly located, and cause fewer neurological symptoms but encase the subclavian vessels. If there is evidence of invasion of the vertebral body or spinal canal, encasement of the subclavian vessels, or unequivocal involvement of the superior branches of the brachial plexus (C8 or above), the tumour is then classified as T4. Direct extension to parietal pericardium is classified T3 and to visceral pericardium, T4. The uncommon superficial spreading tumour of any size with its invasive component limited to the bronchial wall, which may extend proximal to the main bronchus, is clas sified as T1a. The classification of additional tumour nodules in lung cancer depends upon their histological appearances. If limited to the lobe of the primary tumour such tumours are classified as T3, when found in other ipsilateral lobes are designated as T4 and if found in the contralateral lung are designated M1a. Multiple tumours of similar histological appearance should only be considered to be synchronous primary tumours if in the opinion of the pathologist, based on features such as diferences in morphology, immunohistochemistry and/ or molecular studies, or, in the case of squamous cancers, are associated with carcinoma in situ, they represent dif fering sub-types of the same histopathological cell type. These circumstances are most commonly encountered when dealing with either bronchioloalveolar carcinomas or adenocarcinomas of mixed subtype with a bronchioloalveolar component. The highest T category and stage of disease should be assigned and the multiplicity or the number of tumours should be indicated in parenthesis. This distinction may require histopathological confirmation of cell type from more than one tumour nodule, where clinically appropriate. In the above classification lung difers from other sites in the application of General Rule 5 as the classification of addi tional tumour nodules applies not only to grossly recognizable tumours but also those that are microscopic or otherwise only discovered on pathological examination, a not unusual finding in lung cancer. However, if such inva sion is clearly limited to fat within the hilum, classification as T2a or T2b is appropriate, depending upon size, unless other features dictate a higher T category. The regional lymph nodes are the intrathoracic, scalene, and supraclavicular nodes. In this nomen clature ipsilateral or contralateral node involvement in #1 would be classified as N3. Involvement of mediastinal nodes, if limited to the midline stations or ipsilateral stations (#2-9), would be classified as N2. Direct extension of the primary tumour into lymph nodes is classified as lymph node metastasis. An exploratory analysis suggested that nodal extent could be grouped into three categories with difering prognoses: i) involvement of a single N1 zone, designated as N1a, ii) involvement of more than one N1 zone, designated as N1b, or a single N2 zone, designated N2a, and iii) involvement of more than one N2 zone, desig nated as N2b. It was suggested that radiologists, clinicians and oncologists use the classification prospectively, where more detailed data on nodal stations is not available, to assess the utility of such a classification for future revision. Nodal station Description Definition #1 Low cervical, Upper border: lower margin of cricoid (Lef/ supraclavicular cartilage Right) and sternal Lower border: clavicles bilaterally and, notch nodes in the midline, the upper border of the manubrium #L1 and #R1 limited by the midline of the trachea. The survival analyses performed on patients whose tumours were resected and had an adequate intraoperative nodal evaluation revealed four categories with diferent prog nosis: i) involvement of a single N1 station, designated as N1a, ii) involvement of more than one N1 station, designated as N1b, or involvement of one N2 station without N1 disease (skip metasta sis), designated as N2a1, iii) involvement of one N2 station with N1 disease, designated as N2a2, and iv) involvement of more than one N2 station, designated N2b. From the analyses of nodal zones and stations, it is evident that the amount of nodal dis ease has prognostic impact. It is suggested that quantification of nodal disease be made with the available methods at clini cal staging, and with systematic nodal dissection at the time of lung resection, either open or video-assisted. Quantifying nodal disease assists physicians in refining prognosis, and in planning therapy and follow-up. Pleural/pericardial efusions are classified as M1a, Most pleural (pericardial) efusions with lung cancer are due to tumour. In a few patients, however, multiple microscopi cal examinations of pleural (pericardial) fluid are negative for tumour, and the fluid is non-bloody and is not an exu date. Where these elements and clinical judgment dictate that the efusion is not related to the tumour, the efusion should be excluded as a descriptor. Tumour foci in the ipsilateral parietal and visceral pleura that are discontinuous from direct pleural invasion by the primary tumour are classified M1a. Pericardial efusion/pericardial nodules are classified as M1a, the same as pleural efusion/nodules. Distant metastases are classified as M1b if single and M1c if multiple in one or in several organs. Discontinuous tumours outside the parietal pleura in the chest wall or in the diaphragm are classified M1b or M1c depending on the number of lesions. In cases classified as M1b and M1c due to distant metasta ses it is important to document all of the sites of metastatic disease, whether the sites are solitary or multiple and in addi tion if the metastases at each site are solitary or multiple. For this reason the V classification is applicable to indicate vascu lar invasion, whether venous or arteriolar. The former categories limited and extensive for small cell carcinoma have been inconsistently defined and used. R1(is) the requirements for R0 have been met, but in situ carcinoma is found at the bronchial resection margin. If resection has been performed, and otherwise fulfils the requirements for complete resection, it should be classified as R0. A new category, R0(un), is proposed to document those other features that fall within the proposed category of uncer tain resection, i. Impact of genetic, clinical and radiologic advances since the 2004 classification. Impact of positive pleural lavage cytol ogy on survival of patients having lung resection for non-small-cell lung cancer: An international individual patient data meta-analysis. However, adequate N staging is generally considered to include sampling or dissection of lymph nodes from stations 2R, 4R, 7, 10R and 11R for right-sided tumours, and stations 5, 6, 7, 10L and 11L for lef-sided tumours. The more peripheral lymph nodes at stations 12-14 are usually evaluated by the pathologist in lobectomy or pneumonectomy specimens but may be separately removed when sublobar resections. Three of these nodes/ stations should be mediastinal, including the subcarinal nodes (#7) and three from N1 nodes/stations. If all resected/sampled lymph nodes are negative, but the number recommended is not met, classify as pN0. If resection has been performed, and otherwise fulfils the requirements for complete resection, it should be classified as R0. At pathological examination, the solid component usually cor responds to the invasive part; and the ground glass opacity, to the lepidic part. However, documentation of both the size of the solid component/invasive part and of the whole tumour including the ground glass and lepidic com ponents in radiology and pathology reports, respectively, is recommended. The clinical and pathological criteria to diferentiate second primary from related tumours are defined in Table 5. Classification depends on the location of the separate tumour nodule(s): T3 if the separate tumour nodule(s) is(are) in the same lobe of the primary tumour; T4, if located in a diferent ipsilat eral lobe; M1a, if located in the contralateral lung. If there are additional extrathoracic metastases, the tumour will be classified as M1b or M1c depending on the number of metastatic sites. The clinical and pathological criteria to categorise separate tumour nodules (intrathoracic metas tasis) are defined in Table 5. Regardless of the location of the tumours, the rule of the highest T with the number (#) or (m) for multiple in parentheses, and an N and an M for all of the multiple tumours collectively applies for these tumours.
Trusted meldonium 250 mg. Flu Attack! How A Virus Invades Your Body | Krulwich Wonders | NPR.