Jonathon D. Truwit MD
- Senior Associate Dean for Clinical Affairs
- E. Cato Drash Professor of Medicine
- Pulmonary and Critical Care Medicine
- University of Virginia Health System
- Charlottesville, VA, USA
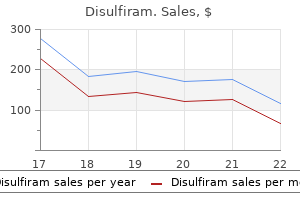
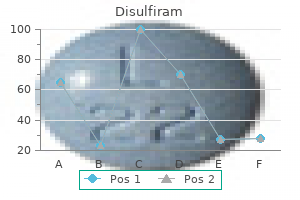
In the early stages symptoms 9 days after ovulation discount disulfiram 500mg without a prescription, patients show a thickening of the nail tablets medications list a-z generic 500 mg disulfiram with visa, which have a rough surface medications questions generic 500mg disulfiram with mastercard. Congenital malalignment of the big toenail is a lateral deviation of the nail plate of both big toenails (Figure 9 treatment lice generic disulfiram 250mg online. If spontaneous recovery does not occur treatment uti purchase 250mg disulfiram otc, surgical intervention may be proposed to realign the nails aquapel glass treatment buy discount disulfiram 250mg on-line. Supernumerary or Ectopic Nails (Onychoheterotopia) A nail is not in its usual location. These are sporadic cases, but two familial cases have been reported; some are associated with chromosomal abnormalities. Then, from approximately two years of age, angiofbroma papules appear on the face, with hypomelanotic macules or shagreen patches. Cardiac problems and renal tumors can be associated with this condition as well as mental retardation. Firm masses, ovoid, white or pinkish, that may appear from the nail folds are Koenen tumors. They appear under the proximal nail fold or under a side fold on the fngers or toes. They usually result in a longitudinal leuconychia, splinter hemorrhage, canaliform depression, or groove of the nail plate (Figure 9. No nail deformity occurs after excising the tumor after total removal of the nail temporarily. Nail Hamartomas 111 Subungual Exostosis A bone exostosis is a benign solitary lesion. It is characterized by a growing mass of hyaline cartilage, then lamellate trabecular bone (Figure 9. Multiple exostosis syndrome16 is rare, familial, with autosomal dominant inheritance. Painful Subungual Tumor in Incontinentia Pigmenti the condition is very rare and found late in life. Histologically, the epidermis is hyperplastic, made of glassy keratinized keratinocytes. Peripheral Nerve Hamartoma with Macrodactyly of the Hand (Peripheral Lipofibromatous Hamartoma of the Median Nerve) Hamartomas of the median nerve or its branches cause congenital macrodactyly, called nerve territory oriented macrodactyly, also called lipofbromatous hamartoma. A woman presented asymp tomatic nodules on the hand and foot, frst developed around the age of 12 years. Histologically, proliferation of eccrine sweat glands and capillaries in close association was observed. Epidermal nevus syndrome is considered when extracutaneous lesions are associated with an epidermal nevus. Some of the lesions are congenital, but a number on the lines of Blaschko occur secondarily. It features a thinned nail, breaking on a ridge, split longitudi nally, transverse, or leukonychia punctuated with onycholysis, and a longitudinal red band. Nail Hamartomas 113 Neurofibromatosis Subungual neurofbromas can occur as isolated elements or associated with a known neurofbromatosis. However, most cases are of sporadic occur rence, corresponding to a new mutation. Tricho-Rhino-Phalangeal Syndrome the main features are bright and sparse hair, a bulbous nose, an elongated philtrum, and abnormalities of the fngers. The characteristic signs are oral leukoplakia, poikiloderma of the sides of the neck, dystrophic nails with cracked to irregular surface, resulting in an almost complete atrophy of the nails. Lethal Hamartoma Syndromes Aplasia or hypoplasia of the nails is part of the array of several genetic diseases exceptionally observed, which generally include abnormalities of the fngers. Multiple ungueal fbromas as an only cutaneous manifestation of tuberous sclerosis complex. Evaluation of the nail changes after surgical excision through the nail bed for subungual glomus tumor. Diagnosis, management, and complications of glomus tumors of the digits in neurofbromatosis type 1. Exostoses sous-ungueales des doigts au cours de la maladie exosto sante hereditaire. Peripheral nerve hamartoma with macrodactyly in the hand: Report of three cases and review of the literature. Rapp-Hodgkin syndrome: An ectodermal dysplasia involv ing the teeth, hair nails, and palate. Vascular tumors are divided into benign, locally aggressive, and malig nant entities, hemangiomas being the most frequent benign vascular tumor in childhood. Their classifcation is based on vessel types that are involved (capillary, venous, lymphatic, lymphedema, and arteriovenous). They were more likely to be segmental and to be of minimal arrested growth type, more than half of them having a predominantly reticular morphology. In only 5% of cases, there was an involvement of some fngertips or toes and sparing of others. Localization under the proximal nail fold has very rarely been reported in the avail able literature. The vascular proliferation produced a reddish discoloration of the nail, which typically faded with compression. Note that the infantile hemangioma spares the extremities of four of the digits but involves the nail matrix as well as the nail bed of the great toe. They are composed of benign spindle cells, which may protrude into the lumen of larger vessels. The location and hematological effects of the lesion may determine whether the treatment is medical or surgical. They are borderline between benign hemangiomas and angiosarcomas, having a tendency to recur but a limited capacity to metastasis. Radiographs showed a combination of lytic destruction and irregular sclerotic changes. Angiogram showed staining of the tumor, early venous flling, and an arteriovenous shunt, suggesting that the tumor was hypervas cular. Other drug-induced cases such as systemic etretinate, systemic acitretin, antiretrovirals (indinavir, lamivudine), or antineoplastic drugs (epidermal growth factor receptor inhibitors, capecitabine, cyclosporin, docetaxel, mitoxantrone) are rarely seen in 120 Pediatric Nail Disorders childhood. Therapy should be as simple as possible to avoid disfguring scars or nail deformity. They can sometimes partially lighten during the frst weeks of birth, the darker aspect at birth being probably due to physiological polyglobulia and relative neonatal cyanosis. However, they generally per sist throughout life and they may even thicken and darken with time. Involvement of the tips of the fngers or nails has not been specifcally described in the literature but can occur. They are round, oval, or with irregular borders and are often surrounded by a pale halo. Patients also have zones of numerous punctuate red spots surrounded by a white halo, located mainly on the extremities. Associated fast-fow lesions can be cutaneous, subcutaneous, intramuscular, intraosseous, intracerebral, or intraspinal. The distal phalanges are hypoplastic with hypoplasia or aplasia of one or several toenails. The lesions are usually present at birth and preferentially involve the lower limbs, followed by the trunk and face. The defects involve more often the lower limbs and characteristically affect the distal phalanges or entire digits. They can become extensive causing chronic complications such as pain, bleeding, functional impairment, and local thrombosis. Because of slow fow of blood into the malformed vessels, thrombosis may occur, resulting in pain and formation of phleboliths that may be palpable or visible on imaging when calcifed. They differ from solitary glomus tumors that are subungual, painful lesions exclusively composed of glomus cells without a major vascular component. The nodules had been present since birth, and they had increased in size during childhood. In addition, she had temporal triangular alopecia, heterochromia irides, epidermal nevus, and lipoblastoma. Puberty and trauma may trigger growth making the fast-fow nature clinically evident. The veins become prominent on the fngers and dorsum of the hand or foot (Figure 10. Intervention may become necessary when local complications such as ulceration, necrosis, pain, bleeding, dimin ished function, or a combination of these occur. They may occur in various sites, cutaneous or visceral, but the most common location is the scalp. The bones of the upper extremity and the max illofacial region are the predominant osseous locations of the disease. A few cases have been described with metacarpal or metatarsal involvement, but the phalanges were rarely or minimally affected. It is characterized by lower limb lymphedema, present as pedal edema at (or before) birth, or develops soon after. Other features sometimes associated with Milroy disease include hydrocele (37% of males), prominent veins (23%), papillomatosis (10%), and urethral abnormalities in males (4%). Individual manifestations can appear at dif ferent times, thus clinical onset varies from birth to late adult life. Nail dystrophy observed in both the lymphedematous and the unaffected lower limb in each of the four children constitutes part of the syndrome. These non vascular anomalies are often overgrowth of soft tissue and/or bone or, rarely, undergrowth. These abnormalities include thick nails, thin nails, brachyonychia, koilonychia, and bluish nails. Anomalies of the extremities such as macrodactyly, clinodactyly, ectrodactyly, camptodactyly, and syn dactyly have been described. It manifests before the completion of 1 year in 25% of patients and by puberty in 80%. Cutaneous and bone lesions may result in gross deformity of the fngers and nail regions. The most frequent location for enchondromas is the small bones of the hands and feet. Involvement of the short tubular bones in the extremities is common; in one-half of patients, bone lesions are unilateral with develop ment of notable malformations. Histopathologically, it is characterized by the proliferation of small vessels in the dermis and subcutane ous tissue; the superfcial epidermis usually shows a papillary appearance with ectatic vessels mimick ing angiokeratomas. They range from skin-colored Vascular Anomalies of Nail and Finger Extremities 129 papules and nodules to more vesicular and bullous-appearing erythematous and violaceous lesions that can be in groups or arranged in a linear fashion. Vascular anomalies clas sifcation: Recommendations from the International Society for the Study of Vascular Anomalies. Multifocal lymphangioendotheliomatosis with thrombocytope nia: A newly recognized clinicopathological entity. Capillaroscopy of the dorsal skin of the hands in hereditary hemorrhagic telangiectasia. The wide spectrum of clinical expression in Adams-Oliver syn drome: A report of two cases. Changes in the nail unit in patients with secondary lymph oedema identifed using clinical, dermoscopic, and ultrasound examination. Possible new autosomal recessive syndrome of congenital lymph oedema, nail dystrophy and esotropia in a Saudi family. Cutaneous manifestations of Proteus syndrome: Correlations with general clinical severity. Foot or hand malformations related to deep venous system anomalies of the lower limb in Klippel-Trenaunay syndrome. Linear acral pseudolymphomatous angiokeratoma of children with associated nail dystrophy. In all these cases, assessing the casual relationship with the systemic disease is not easy. This chapter describes clubbing in association with several disorders in children and then reviews the systemic diseases of children that have been associated with nail lesions. It is characterized by a focal bulbous enlargement of the terminal segments of the fngers and/or toes that produce an alteration of the shape of the nail, which resembles a clock glass, being hypercurved both transversally and longitudinally. On palpation, the enlarged tissues of the proximal nail fold have a spongy sensation. Although the severe clubbing is recognized very easily, the identifcation of the early stages can be diffcult.
Although there is no evidence of adverse fetal effects from vaccinating pregnant women with an inactivated virus or bacterial vaccines or toxoids medications while pregnant buy discount disulfiram 500mg, ideally vac cinations should be administered before conception in order to avoid unneces sary exposure to the fetus treatment 11mm kidney stone order cheap disulfiram. Women who receive a live-virus vaccination should be advised to avoid preg nancy for at least 1 month after vaccination treatment jalapeno skin burn purchase disulfiram line. No study to date has shown an adverse consequence of the inactivated influenza vaccine in preg nant women or their offspring medicine man aurora generic disulfiram 250 mg otc. Vaccination early in the season and regardless of gestational age is optimal treatment 3 antifungal 500mg disulfiram with amex, but unvaccinated pregnant women should be immu nized at any time during the influenza season as long as the vaccine supply lasts symptoms celiac disease generic disulfiram 500mg otc. In addition, women who have not been immunized with the tetanus toxoid, Preconception and Antepartum Care 99 reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) or women whose vaccine status is unknown should be offered immunization with Tdap. In addition, vaccination(s) should be offered to women found to be at risk of or susceptible to measles, mumps, rubella, varicella, hepatitis A, hepatitis B, meningococcus, and pneumococcus. However, because the vaccine is not recommended during pregnancy, comple tion of the vaccine series may need to be delayed until the postpartum period. Sexually Transmitted Infections Chlamydia trachomatis and Neisseria gonorrhea have been strongly associated with ectopic pregnancy, infertility, and chronic pelvic pain. Annual screening of chlamydial infection for all sexually active women aged 25 years or younger is recommended, as is screening of older women with risk factors (eg, those who have a new sex partner or multiple sex partners). Syphilis during pregnancy might result in fetal death or substantial physical and developmental disabilities, including intellectual disabilities and blindness. Substance Use and Abuse Behavioral counseling can be particularly effective during the preconception period and antenatal period. Preconception women who smoke cigarettes or use any other form of tobacco product should be identified and encouraged and supported in an effort to quit. Importantly, tobacco cessation at any point during pregnancy yields substantial health benefits for the expectant mother and newborn. There is a strong association between smoking during pregnancy and sudden infant death syndrome. Children born to mothers who smoke dur ing pregnancy are at increased risk of asthma, infantile colic, and childhood obesity. Patients who 100 Guidelines for Perinatal Care are willing to try to quit smoking benefit from a brief counseling session, such as the 5-A intervention (Box 5-1), which has been proven to be effective when initiated by health care providers. Other important behavioral issues to address include alcohol use and mis use and the abuse of prescription and nonprescription recreational drugs. Women who are trying to become pregnant should be counseled to completely refrain from all alcohol use. Referral relationships with appropriate resources should be established and used as needed to assist women with these issues. Women who are counseled concerning their alcohol or drug use should be fol lowed up to assess adherence to recommendations. It has been shown that achieving preconception and early pregnancy blood sugar control can decrease the risk of spontaneous abortion, birth defects, and macrosomia. Preconception and Antepartum Care 101 thyroidism should be appropriately treated so that they are euthyroid before attempting pregnancy. Inadequately treated hyperthyroidism or hypothyroid ism is associated with adverse pregnancy outcomes, including miscarriage and preterm delivery. Other chronic medical conditions that should be addressed preconceptionally include asthma, hemoglobinopathies, inherited thrombophilias, obesity, a history of bariatric surgery, and hyperten sion. In general, using the lowest effective dose of only necessary medications is recommended. Some common teratogenic medications include the oral anticoagulant warfarin, the antiseizure drugs valproic acid and carbamazepine, isotretinoin, and angiotensin-converting enzyme inhibitors. Preconception Genetic Screening Preconception visits are a reasonable time to offer screening for genetic disorders based on racial and ethnic background. Testing both partners preconception ally is often more straightforward and less stressful than doing so in pregnancy, although insurance carriers may decline to reimburse for this testing. Physicians also may perform preconception screening for other genetic disorders on the basis of family history (eg, fragile X syndrome for individuals with a family history of nonspecific, predominantly male-affected mental retar dation; Duchenne muscular dystrophy). Women who frequently diet to lose weight, fast, skip meals, or have eating disorders or unusual eating habits should be identified and counseled. Additional risk factors for nutritional problems include adolescence, tobacco and substance abuse, history of pica during a previous pregnancy, high parity, and mental illness. Women who have undergone bariatric surgery should be assessed as well because some of these surgical procedures affect vitamin absorp tion and B12 production. All women should be encouraged to exercise at least 30 minutes on most days of the week. Obese women should be advised regarding their increased risk of adverse perinatal outcomes, including difficulty becoming pregnant, conception of a fetus with a variety of birth defects, preterm delivery, diabetes, cesarean delivery, hyperten sive disease, and thromboembolic disease. Dietary supplements are particularly important during the preconception period (Table 5-2). Public Health Service recommend the daily intake of 400 micrograms of folic acid for all women who could become pregnant. Public Health Service guideline, which recommends the daily consumption of 4,000 micrograms of folic acid beginning 1 month before trying to conceive and continuing through the first 3 months of pregnancy. Preconception and Antepartum Care 105 Women also should assess their diets and dietary supplements to confirm that they are meeting the recommended daily doses for calcium, iron, vitamin D, vitamin A, vitamin B12, and other nutrients, minerals and vitamins (Table 5-2). Department of Health and Human Services recommend that women who could become pregnant consume foods that supply heme iron (which is more readily absorbed by the body), additional iron sources, and foods that enhance iron absorption, such as those rich in vitamin C (eg, citrus fruits, strawberries, broccoli, and tomatoes). Antepartum Care Women who receive early and regular prenatal care are more likely to have healthier infants. Prenatal care includes a process of ongoing risk identification and assessment in order to develop appropriate care plans. This plan of care 106 Guidelines for Perinatal Care should take into consideration the medical, nutritional, psychosocial, cultural and educational needs of the patient and her family, and it should be periodi cally reevaluated and revised in accordance with the progress of the pregnancy. Health care providers of antepartum care must be able to either primarily provide or easily refer to others to provide a wide array of services to pregnant women. Prenatal Care Visits the first visit for prenatal care typically occurs in the first trimester. The fre quency of follow-up visits is determined by the individual needs of the woman and an assessment of her risks. Women with poor pregnancy outcomes in earlier pregnancies, known medical problems, vaginal bleeding before initiation of routine prenatal care, and those who achieved a pregnancy through infertility treatments and are known to be carrying multiple gestations should be seen as early as possible. Typically, a woman with an uncomplicated first pregnancy is examined every 4 weeks for the first 28 weeks of gestation, every 2 weeks until 36 weeks of gestation, and weekly thereafter. Women with medical or obstetric prob lems, as well as women at the extremes of reproductive age will likely require close surveillance; the appropriate intervals between scheduled visits are deter mined by the nature and severity of the problems (see also Appendix B and Appendix C). Likewise, parous women with prior normal pregnancy outcomes and without medical and obstetric problems during the current pregnancy may Preconception and Antepartum Care 107 be able to be seen less frequently as long as additional visits on an as-needed basis are available. Appendix A contains a format for documenting information and the database recommended by the American College of Obstetricians and Gynecologists (the College). Whatever format is used, the record should be designed to record the large amount of data in a lon gitudinal manner that is clear and concise, to prompt the health care provider to complete the evaluations and screening steps appropriate for that patient, and to communicate the results in a clear fashion to the users of the chart. After the patient reports quicken ing and at each subsequent visit, she should be asked about fetal movement. She should be queried about contractions, leakage of fluid, or vaginal bleeding, the time-honored inclusion of routine urine dipstick assessment for all pregnant women can be modified according to site-specific protocols. A base line screen for urine protein content to assess renal status is recommended. However, in the absence of risk factors for urinary tract infections, renal disease, and preeclampsia (such as diabetes, hypertension, and autoimmune disorders) and in the absence of symptoms of urinary tract infection, hypertension or unusual edema, there has not been shown to be a benefit in routine urine dip stick testing during prenatal care for women at low risk. Group Prenatal Care Group, or shared, medical visits have been in use in a variety of medical settings during the past two decades and have been associated with improved health outcomes for patients. Currently, there are several models of group prenatal care in use that show promise. Preconception and Antepartum Care 109 In group prenatal care, health care providers deliver prenatal health services and information to groups of patients during regularly scheduled shared vis its. The group visits are begun after the first prenatal assessment and physical examination, and groups usually comprise women with similar estimated deliv ery dates. Health care providers are assisted by a variety of other health care professionals, who may serve as a co-facilitator or a guest for a specific topic. The group model is a promising innovation in prenatal care delivery, but additional research and evaluation of patient outcomes are needed. Practitioners should approach group prenatal care with deliberate planning and research. In addition to the planning aspects for the pregnant woman herself, this information is vital for the scheduling and interpretation of certain antepartum tests, determination of appropriateness of fetal size estimates in order to risk-assess accurately, and designing interventions to prevent preterm births, postterm births, and related morbidities. The first date of the last menstrual period, when known, should be recorded in the chart, as well as documentation regarding the reliability of this date. Factors, such as maternal uncertainty, use of hormonal contraceptives within the past 6 months, irregular cycles, and recent pregnancy or lactation should be noted. In general, ultrasound-established dates should take preference over menstrual dates when the discrepancy is greater than 7 days in the first trimes ter and greater than 10 days in the second trimester. Once the dates are established by a last menstrual period with consistent ultrasound examina tion or an early ultrasonography alone, the final estimated delivery date should 110 Guidelines for Perinatal Care not be altered. Fetal Ultrasound Imaging Ultrasonography is the most commonly used fetal imaging tool and is an accurate method of determining gestational age, fetal number, viability, and placental location. Ultrasonography should be performed only by technologists or physicians who have undergone specific training and only when there is a valid medical indication for the examination. Physicians who perform, evaluate, and interpret diagnostic obstetric ultrasound examinations should be licensed medical practitioners with an understanding of the indications for such imag ing studies, the expected content of a complete obstetric ultrasound examina tion, and a familiarity with the limitations of ultrasound imaging. A physician is responsible for the interpretation of all studies; ultrasonographers may not interpret the studies nor bill for them. The timing and type of ultrasonography performed should be such that the clinical question being asked is answered. In order to select the best time for a particular patient to receive her scan, health care providers must balance the types and accuracy of information to be gained at different gestational ages with the financial reality of limitations to the number of scans many insurance carriers will pay for. Each type of ultrasound examination should be performed only when indi cated and should be appropriately documented. A first-trimester ultrasound examination is an ultrasound examination performed before 13 weeks and 6 days of gestation. Scanning in the first trimester can be performed transab dominally or transvaginally. Indications for performing first-trimester ultra sound examinations are listed in Box 5-2. Second-trimester and third-trimester ultrasound examinations include the following three types: 1. Patients with an abnormal fetal ultrasound examination result should be referred for evaluation and management of fetal anomalies to a health care provider who can accurately and thoroughly assess the fetus, communicate the findings to the patient and health care provider, and coordinate further man agement if needed. Fetal Magnetic Resonance Imaging If additional imaging modalities are required prenatally, magnetic resonance imaging may be chosen. The most common use of fetal magnetic resonance imag ing is to further delineate a fetal anomaly or rule out placenta accreta identified or suspected on ultrasound examination results. Although the safety of ultra sonography has been established, comparatively few studies have analyzed the safety of magnetic resonance imaging; however, this technology is being used with increasing frequency in pregnant patients, and there are no known risks.
Buy disulfiram 500 mg visa. The Treatment of Multiple Sclerosis - Signs of Multiple Sclerosis Therapy.
Plan the key steps and know the potential pitfalls in performing umbilical vessel catheterization c medications hyperkalemia purchase disulfiram with amex. Know the anatomy and pathophysiology relevant to umbilical vessel catheterization 4 symptoms irritable bowel syndrome cheap disulfiram. Know the anatomy and pathophysiology relevant to emergency management of congenital anomalies b medicine 751 m disulfiram 500mg mastercard. Know the indications and contraindications for emergency management of congenital anomalies c symptoms estrogen dominance purchase on line disulfiram. Plan the key steps and know the potential pitfalls in the emergency management of congenital anomalies d medications ocd buy 250 mg disulfiram with amex. Recognize the complications associated with the emergency management of congenital anomalies F symptoms 4 days before period generic disulfiram 500mg free shipping. Plan the key steps and know the potential pitfalls in performing lumbar puncture c. Know the indications and contraindications for ventricular shunt and burr hole puncture b. Plan the key steps and know the potential pitfalls in performing ventricular shunt and burr hole puncture c. Recognize the complications associated with ventricular shunt and burr hole puncture d. Know the anatomy and pathophysiology relevant to ventricular shunt and burr hole puncture 3. Plan the key steps and know the potential pitfalls in performing ventricular puncture d. Know the indications and contraindications for general pediatric ophthalmic procedures b. Plan the key steps and know the potential pitfalls in performing general pediatric ophthalmic procedures c. Recognize the complications associated with general pediatric ophthalmic procedures d. Know the anatomy and pathophysiology relevant to general pediatric ophthalmic procedures 2. Plan the key steps and know the potential pitfalls in performing slit lamp examination c. Plan the key steps and know the potential pitfalls in performing ocular foreign body removal c. Know the indications and contraindications for ocular irrigation and decontamination b. Plan the key steps and know the potential pitfalls in performing ocular irrigation and decontamination c. Recognize the complications associated with ocular irrigation and decontamination d. Know the anatomy and pathophysiology relevant to ocular irrigation and decontamination 5. Know the anatomy and pathophysiology relevant to eye patching and eye guard application b. Know the indications and contraindications for eye patching and eye guard application c. Plan the key steps and know the potential pitfalls in performing eye patching and eye guard application d. Recognize the complications associated with eye patching and eye guard application 6. Plan the key steps and know the potential pitfalls in performing contact lens removal c. Know the anatomy and pathophysiology relevant to acute upper airway foreign body removal b. Know the indications and contraindications for acute upper airway foreign body removal c. Plan the key steps and know the potential pitfalls in performing acute upper airway foreign body removal d. Recognize the complications associated with acute upper airway foreign body removal 2. Plan the key steps and know the potential pitfalls in performing otoscopic examination d. Plan the key steps and know the potential pitfalls in performing removal of impacted cerumen c. Know the indications and contraindications for foreign body removal from the external auditory canal b. Plan the key steps and know the potential pitfalls in performing foreign body removal from the external auditory canal c. Recognize the complications associated with foreign body removal from the external auditory canal d. Know the anatomy and pathophysiology relevant to foreign body removal from the external auditory canal 5. Plan the key steps and know the potential pitfalls in performing external ear procedures c. Plan the key steps and know the potential pitfalls in performing tympanocentesis c. Know the indications and contraindications for drainage and packing of a nasal septal hematoma b. Plan the key steps and know the potential pitfalls of draining and packing a nasal septal hematoma c. Recognize the complications associated with drainage and packing of a nasal septal hematoma d. Know the anatomy and pathophysiology relevant to drainage and packing of a nasal septal hematoma 9. Plan the key steps and know the potential pitfalls in performing nasal foreign body removal 10. Plan the key steps and know the potential pitfalls in performing pharyngeal procedures c. Know the indications and contraindications for direct and indirect diagnostic laryngoscopic procedures b. Know the anatomy and pathophysiology relevant to direct and indirect diagnostic laryngoscopic procedures c. Plan the key steps and know the potential pitfalls in performing direct and indirect diagnostic laryngoscopic procedures d. Recognize the complications associated with direct and indirect diagnostic laryngoscopic procedures I. Know the anatomy and pathophysiology relevant to orofacial anesthesia techniques b. Plan the key steps and know the potential pitfalls of orofacial anesthesia techniques d. Know the anatomy and pathophysiology relevant to incision and drainage of a dental abscess b. Know the indications and contraindications for incision and drainage of a dental abscess c. Plan the key steps and know the potential pitfalls in performing incision and drainage of a dental abscess d. Recognize the complications associated with incision and drainage of a dental abscess 3. Know the anatomy and pathophysiology relevant to management of dental fractures b. Plan the key steps and know the potential pitfalls in managing dental fractures d. Know the indications and contraindications for reimplanting an avulsed permanent tooth b. Plan the key steps and know the potential pitfalls in reimplanting an avulsed permanent tooth c. Recognize the complications associated with reimplanting an avulsed permanent tooth d. Know the anatomy and pathophysiology relevant to reimplanting an avulsed permanent tooth 5. Plan the key steps and know the potential pitfalls in application of a dental splint c. Know the anatomy and pathophysiology relevant to application of a dental splint 6. Know the anatomy and pathophysiology relevant to management of soft tissue injuries of the mouth b. Know the indications and contraindications for management of soft tissue injuries of the mouth c. Plan the key steps and know the potential pitfalls in performing management of soft tissue injuries of the mouth d. Recognize the complications associated with management of soft tissue injuries of the mouth 7. Know the anatomy and pathophysiology relevant to reduction of temporomandibular joint dislocation b. Know the indications and contraindications for reduction of temporomandibular joint dislocation c. Plan the key steps and know the potential pitfalls in reducing temporomandibular joint dislocation d. Recognize the complications associated with reduction of temporomandibular joint dislocation J. Know the anatomy and pathophysiology relevant to converting stable supraventricular tachycardia using vagal maneuvers b. Know the indications and contraindications for converting stable supraventricular tachycardia using vagal maneuvers c. Plan the key steps and know the potential pitfalls in converting stable supraventricular tachycardia using vagal maneuvers d. Recognize the complications associated with converting stable supraventricular tachycardia using vagal maneuvers 3. Know the indications and contraindications for arterial puncture and catheterization b. Know the anatomy and pathophysiology relevant to arterial puncture and catheterization c. Recognize the complications associated with arterial puncture and catheterization d. Plan the key steps and know the potential pitfalls in performing arterial puncture and catheterization 5. Know the indications and contraindications for venipuncture and peripheral venous access b. Know the anatomy and pathophysiology relevant to venipuncture and peripheral venous access c. Recognize the complications associated with venipuncture and peripheral venous access d. Plan the key steps and know the potential pitfalls in performing venipuncture and peripheral venous access 6. Know the anatomy and pathophysiology relevant to accessing indwelling central catheters b. Know the indications and contraindications for accessing indwelling central catheters c. Plan the key steps and know the potential pitfalls in accessing indwelling central catheters d. Recognize the complications associated with accessing indwelling central catheters K. Plan the key steps and know the potential pitfalls in performing pulse oximetry 2. Plan the key steps and know the potential pitfalls in performing peak flow rate measurement 4. Know the anatomy and pathophysiology relevant to the use of metered dose inhalers, spacers, and nebulizers b. Know the indications and contraindications for the use of metered dose inhalers, spacers, and nebulizers c. Plan the key steps and know the potential pitfalls in the use of metered dose inhalers, spacers, and nebulizers d. Recognize the complications associated with the use of metered dose inhalers, spacers, and nebulizers 5. Know the indications and contraindications for replacement of a tracheostomy cannula b. Know the anatomy and pathophysiology relevant to replacement of a tracheostomy cannula c. Plan the key steps and know the potential pitfalls in replacing a tracheostomy cannula 7. Plan the key steps and know the potential pitfalls in performing mechanical ventilation d. Plan the key steps and know the potential pitfalls in performing oral rehydration d. Plan the key steps and know the potential pitfalls in performing gastrostomy tube replacement 4. Plan the key steps and know the potential pitfalls in performing hernia reduction 6. Know the anatomy and pathophysiology relevant to treatment of umbilical granuloma b. Know the indications and contraindications for treatment of umbilical granuloma c.
If the tube is too large treatment 3rd degree hemorrhoids order disulfiram discount, replacing it with a smaller one may resolve the problem medicine 93 3109 order disulfiram 250 mg otc. If there has been significant bleeding symptoms in children purchase genuine disulfiram on-line, gastric lavages are helpful; it is controversial whether tepid water or normal saline is best treatment of criminals buy disulfiram online from canada. This diagnosis is difficult to document treatment xdr tb buy disulfiram 500mg visa, so it is usually made if the patient has remission of symptoms when the formula is eliminated medications ocd order 250 mg disulfiram overnight delivery. Treatment usually consists of ranitidine or cimetidine (for dosages and other pharmacologic information, see Chapter 80). Use of antacids in neonates is controversial; some clinicians believe that concretions may result from the use of antacids. Is the mother too sick or uncomfortable to be able to adequately participate in the discussion In this situation, other family members are essential to participate in the discussion. Although a neonatologist can be called on to counsel expectant parents in a variety of circumstances, the following are common problems that are discussed with parents before delivery. Obtain the following information: age of both parents, obstetric history, history of the current pregnancy, medication history, pertinent laboratory and sonographic data, family history, social background and supports, and communication ability. Review current fetal information with the obstetrician: abnormalities of fetal heart rate and fetal tracing, biophysical profile, fetal scalp pH (if done), and any other pertinent tests. Parent counseling before delivery is often performed under less than ideal circumstances. Every effort should be made to communicate effectively, explaining all medical terms and avoiding abbreviations and percentages as much as possible. Most important, repetition may be necessary in order for parents to comprehend all this information, and an opportunity to review the information should be provided. Specific and detailed survival and outcome statistics are beyond the scope of this book but are contained in neonatal and obstetric textbooks. The more immature the infant, the greater are the risks of death and all the complications of prematurity, health sequelae, and neurodevelopmental disabilities. Current data, drawn from many published outcome studies, are presented in Table 32-1, although quoting percentages to parents should be avoided. This is the most important question because morbidity and mortality are so closely tied to maturity. Both gestational age and birth weight have been used as proxies for maturity in predicting survival and outcome. However, only gestational age is available when counseling parents in labor and delivery. The very reason for preterm delivery affects infant outcome and the likelihood of delaying delivery (eg, delay is contraindicated with suspected chorioamnionitis). Survival at the lower limit of viability requires intubation and mechanical ventilation, but these efforts may merely prolong death. All the complications of prematurity are most common in infants born at the lower limit of viability, and their frequency decreases with increasing gestational age. Complications of prematurity include respiratory distress syndrome, metabolic problems, infection, necrotizing enterocolitis, patent ductus arteriosus, intraventricular hemorrhage, and apnea and bradycardia. Chronic complications include chronic lung disease, periventricular leukomalacia or intraparenchymal cysts, hydrocephalus, poor nutrition, retinopathy of prematurity, and hearing impairment. Although the risk of disability is higher in preterm children than in the general population, the majority of preterm children do not develop a major disability (see Table 32-1), such as cerebral palsy or mental retardation. The frequency of neurodevelopmental disability is highest at the lower limit of viability. Learning disability, attention deficit disorder, minor neuromotor dysfunction, and behavior problems are also more frequent in school-age preterm children than in full-term controls. The normal fetus initially compensates for fetal deprivation of supply, but when these compensatory mechanisms are overwhelmed, progressive damage to fetal organs occurs, leading to fetal death in utero if there is no intervention. Fetal alcohol and fetal hydantoin syndromes are well defined and carry an increased risk of mental retardation but are often difficult to diagnose in the neonatal period. Infants exposed in utero to opiates or cocaine may demonstrate neonatal withdrawal syndrome. These infants will have to be closely observed and may require medications to help them through the withdrawal period. Infants with central nervous system infarctions resulting from cocaine exposure are at risk for cerebral palsy, especially hemiplegia. There are many different signs of fetal distress, including changes in fetal heart rate patterns, fetal reactivity, meconium staining of amniotic fluid, and decreased fetal movements as well as composite fetal measures (eg, biophysical profile). The type, severity, and duration of insult are important for prognosis, but these cannot be accurately determined. Infants with chronic intrauterine hypoxia are at increased risk for persistent pulmonary hypertension and neurodevelopmental disability (whether or not they require extracorporeal membrane oxygenation; see Table 32-1). Infants with severe hypoxic-ischemic encephalopathy who develop a disability tend to have severe multiple disabilities. Nevertheless, the majority of infants who demonstrate signs of fetal distress or acute perinatal depression do not develop hypoxic-ischemic encephalopathy, persistent pulmonary hypertension of the newborn, or neurodevelopmental disability. Sommerfelt K: Long-term outcome for non-handicapped low birth weight infants: is the fog clearing Cyanosis becomes visible when there is more than 3g of desaturated hemoglobin per deciliter. Therefore, the degree of cyanosis will depend on oxygen saturation and hemoglobin concentration. Cyanosis will be visible with much less degree of hypoxemia in the polycythemic compared with the anemic infant. If the infant has increased respiratory effort with increased rate, retractions, and nasal flaring, respiratory disease should be high on the list of differential diagnoses. Cyanotic heart disease usually presents without respiratory symptoms but can have effortless tachypnea (rapid respiratory rate without retractions). Transposition of the great vessels can present without a murmur (approximately 60%). Is the cyanosis continuous, intermittent, sudden in onset, or occurring only with feeding or crying Intermittent cyanosis is more common with neurologic disorders, because these infants may have apneic spells alternating with periods of normal breathing. Continuous cyanosis is usually associated with intrinsic lung disease or heart disease. Cyanosis with feeding may occur with esophageal atresia and severe esophageal reflux. Cyanosis of the upper or lower part of the body only usually signifies serious heart disease. The more common pattern is cyanosis restricted to the lower half of the body, which is seen in patients with patent ductus arteriosus with a left-to-right shunt. Cyanosis restricted to the upper half of the body is seen occasionally in patients with pulmonary hypertension, patent ductus arteriosus, coarctation of the aorta, and D-transposition of the great arteries. An infant of a diabetic mother has increased risk of hypoglycemia, polycythemia, respiratory distress syndrome, and heart disease. Infection, such as that which can occur with premature rupture of membranes, may cause shock and hypotension with resultant cyanosis. Amniotic fluid abnormalities, such as oligohydramnios (associated with hypoplastic lungs) or polyhydramnios (associated with esophageal atresia), may suggest a cause for the cyanosis. Congenital defects (eg, diaphragmatic hernia, hypoplastic lungs, lobar emphysema, cystic adenomatoid malformation, and diaphragm abnormality). Periventricular-intraventricular hemorrhage, meningitis, and primary seizure disorder can cause cyanosis. Neuromuscular disorders such as Werdnig-Hoffmann disease and congenital myotonic dystrophy can cause cyanosis. Respiratory depression secondary to maternal medications (eg, magnesium sulfate and narcotics). Choanal atresia is nasal passage obstruction caused most commonly by a bony abnormality. Other causes are laryngeal web, tracheal stenosis, goiter, and Pierre Robin syndrome. In peripheral cyanosis, the skin is bluish but the oral mucous membranes will be pink. The liver can be enlarged in congestive heart failure and hyperexpansion of the lungs. Check for apnea and periodic breathing, which may be associated with immaturity of the nervous system. Observe the infant for seizures, which can cause cyanosis if the infant is not breathing during seizures. With cyanotic heart disease, the PaO2 most likely will not increase significantly. If the PaO2 rises above 150 mm Hg, cardiac disease can generally be excluded but not always. Failure of PaO2 to rise above 150 mm Hg suggests a cyanotic cardiac malformation, whereas in lung disease the arterial oxygen saturation should improve and go above 150 mm Hg. Draw a simultaneous sample of blood from the right radial artery (preductal) and the descending aorta or the left radial artery (postductal). If there is a difference of >15% (preductal > postductal), then the shunt is significant. It is sometimes easier to place two pulse oximeters on the infant (one preductal-right hand; one postductal-left hand or either foot). To confirm the diagnosis, a spectrophotometric determination should be done by the laboratory. Transillumination of the chest (see p 169) should be done on an emergent basis if pneumothorax is suspected. It can also help diagnose heart disease by evaluating the heart size and pulmonary vascularity. The heart size may be normal or enlarged in hypoglycemia, polycythemia, shock, and sepsis. Increased arterial markings can be seen in truncus arteriosus, single ventricle, and transposition. Increased venous markings can be seen in hypoplastic left heart syndrome and total anomalous pulmonary venous return. It is very helpful in identifying patients with tricuspid atresia; it will show left axis deviation and left ventricular hypertrophy. Echocardiography should be performed immediately if cardiac disease is suspected or if the diagnosis is unclear. Ultrasonography of the head can be performed to rule out periventricular-intraventricular hemorrhage. If a tension pneumothorax is present, rapid needle decompression may be needed (see also p 293). Order stat laboratory tests (eg, blood gas levels, complete blood cell count, and chest x ray film). Treat the infant with methylene blue only if the methemoglobin level is markedly increased and the infant is in cardiopulmonary distress (tachypnea and tachycardia). Administer intravenously 1 mg/kg of a 1% solution of methylene blue in normal saline. It is important to prepare the family in advance, if possible, for the death of an infant and to be ready to answer questions after the event. Early neonatal death describes the death of a live born infant during the first 7 completed days of life. Late neonatal death refers to the death of a live born infant after 7 but before 28 completed days of life. Usually several immediate family members in addition to the parents are present at the hospital. It is good practice to ensure that there is a contact telephone number available for any sick infant. If the family members are not present, telephone contact must be made as soon as possible to alert the family that their infant is dying or has already passed away. The religious needs must be respected and the necessary support provided (eg, priest, rabbi, minister, or pastoral care). Every hospital has pastoral services, and it is useful to inform the minister in advance because some parents may request that their child be baptized before death. It is important to remember that the infant may continue with a gasp reflex for a while even without spontaneous respiration and movement. The heartbeat may be very faint; therefore, auscultation for 2-5 min is advisable. Examination of the infant by the physician to determine death may be done in that same private area, with the family. Much of the equipment (eg, intravenous catheters and endotracheal tubes) may be removed from the infant unless an autopsy is anticipated. In that case, it is best to leave in place central catheters and possibly the endotracheal tube. This type of visual and physical contact is important to begin the grieving process in a healthy manner and try to relieve any future guilt. Parents and immediate family members should be in a quiet, private consultation room, and the physician should calmly explain the cause and inevitability of death. A brief outline of the normal grieving process may be discussed: shock, denial, sadness, anger, and reorganization. Staff must be aware of the additive stress on the parents looking in on a surviving twin. Family members should be asked whether they need any support for transport or funeral arrangements and whether they need a letter to the employer regarding time off from work and so on.